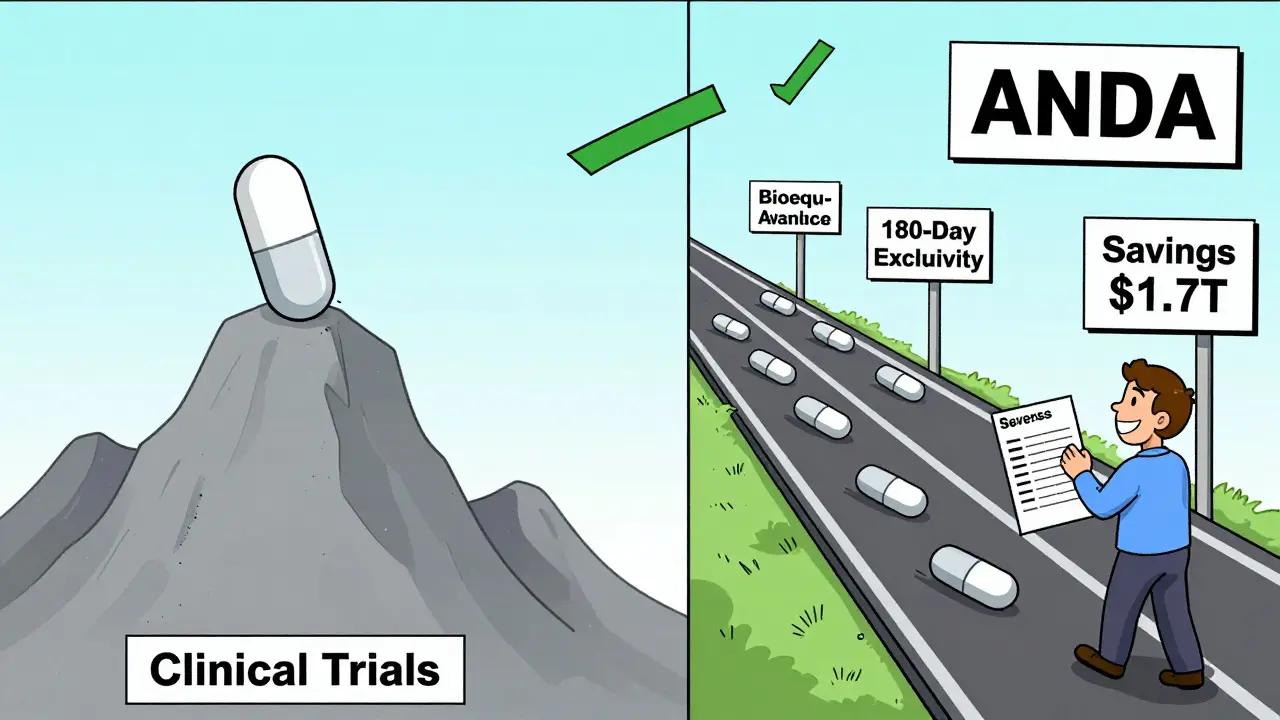
The Hatch-Waxman Act didn’t just change how drugs are approved in the U.S.-it saved trillions. Before 1984, if you wanted to make a generic version of a brand-name drug, you had to start from scratch. That meant running your own clinical trials, even though the original drug had already been proven safe and effective. It cost around $2.6 million just to apply, and approval could take years. Most companies didn’t even try. As a result, when a patent expired, there was often no competition. Prices stayed high. Patients paid more. And the system didn’t work.
What the Hatch-Waxman Act Actually Did
The Drug Price Competition and Patent Term Restoration Act of 1984, better known as the Hatch-Waxman Act, solved this problem by creating a new path: the Abbreviated New Drug Application, or ANDA. This wasn’t a loophole. It was a legal shortcut. Generic manufacturers could now use the FDA’s own findings about the brand-name drug’s safety and effectiveness. All they had to prove was that their version was the same in active ingredient, strength, dosage form, and route of administration. And crucially, that it performed the same way in the body.
That last part-performance-is where bioequivalence comes in. The FDA requires that a generic drug’s absorption into the bloodstream falls within 80% to 125% of the brand-name drug. This isn’t guesswork. It’s measured through blood tests in healthy volunteers. If the numbers match, the drug is considered interchangeable. The FDA doesn’t require another trial on patients. It just needs proof that the body handles the generic the same way.
The Orange Book: The Rulebook for Generic Competition
To make this system work, the Act created the Orange Book. Officially called Approved Drug Products with Therapeutic Equivalence Evaluations, it’s a public list of every approved drug and the patents tied to it. Brand-name companies must list every patent that could block a generic-from the core chemical structure to special coatings or delivery systems. If a patent isn’t listed, it can’t be used to delay generics later.
This transparency changed everything. Generic companies could look up a drug, see which patents were still active, and plan their entry. If a patent had expired, they could file right away. If it was still active, they had to wait-or challenge it.
Paragraph IV: The Game-Changing Challenge
The most powerful tool in the Hatch-Waxman toolkit is the Paragraph IV certification. When a generic company files an ANDA, they must state under oath what they think about each patent listed in the Orange Book. Paragraph IV says: "This patent is either invalid or won’t be infringed by our product."
This is the moment the system gets intense. Filing a Paragraph IV certification triggers a 45-day window for the brand-name company to sue for patent infringement. If they do, the FDA can’t approve the generic for 30 months-unless the court rules sooner. But here’s the catch: if the generic wins that lawsuit, they get 180 days of exclusive market access. No other generic can enter during that time. That’s worth millions. And because of it, companies race to be first.
Some generics have built entire business models around this. Teva, Sandoz, and Mylan (now Viatris) have teams of lawyers and scientists dedicated to finding weak patents and filing Paragraph IV applications before anyone else. In 2023 alone, the FDA approved 746 ANDAs. Roughly 90% of them included Paragraph IV certifications. That’s not coincidence-it’s strategy.
How It Changed the Market
Before 1984, generics made up just 19% of U.S. prescriptions. Today, they make up over 90%. But here’s the real number: while generics account for 90% of prescriptions, they cost only 23% of total drug spending. That’s the power of competition.
When a generic enters, prices don’t just drop-they collapse. A drug that costs $100 per pill might fall to $5 within a year. In some cases, prices drop 80-90%. The Congressional Budget Office estimates that over the last decade, generic drugs saved the U.S. healthcare system $1.7 trillion. Medicare Part D beneficiaries alone save an average of $3,200 per year because of generics.
And it’s not just about money. Access matters. A patient on insulin, statins, or blood pressure meds can now afford their treatment because of this law. Hospitals, pharmacies, and insurers rely on generics to keep costs down. Without Hatch-Waxman, many of these drugs would still be unaffordable.
The Dark Side: Pay-for-Delay and Patent Thickets
It’s not perfect. Brand-name companies have learned to game the system. One tactic is "pay-for-delay"-where a brand pays a generic company to hold off on entering the market. These settlements can delay competition for years. The FTC has challenged dozens of them, but they still happen.
Another problem is "patent thickets"-when a brand files dozens of minor patents on things like pill coatings, packaging, or dosing schedules. These aren’t core inventions. They’re legal fences. The average drug now has 3.5 patents listed in the Orange Book by the time generics enter, up from just 1.5 at launch. That makes it harder for generics to find a clear path.
The FDA has responded. In 2019, Congress passed the CREATES Act, which forces brand companies to provide generic manufacturers with the drug samples they need to test bioequivalence. Before that, some brands refused to sell samples, effectively blocking competition. The FDA now actively enforces this rule.

What’s Next for Generic Drugs?
The Hatch-Waxman Act was built for simple pills. Today, we’re seeing more complex drugs-injectables, inhalers, patches, and even biosimilars-that don’t fit neatly into the ANDA framework. That’s why Congress created the BPCIA in 2010 to handle biologics separately.
But even for small molecules, challenges remain. In 2023, 283 generic drugs faced shortages. Many were old, cheap, and made overseas. Quality control at some factories has been shaky. The FDA’s 2023 Generic Drug User Fee Amendments (GDUFA) III are trying to fix this by speeding up reviews and improving inspections. Review times have dropped from 36 months in 2012 to 18 months in 2023.
Experts agree: the system works-but it’s under strain. More drugs are coming off patent. More complex. More expensive to copy. And more companies are fighting to delay entry. The FDA is adapting. Congress is debating reforms. But the core idea remains: if a drug is safe and effective, let others make it. Let competition drive prices down. Let patients win.
How It Compares to Other Countries
The U.S. system is unique. In Europe, generics can enter right after patent expiry, but there’s no 180-day exclusivity. No legal race. No financial incentive to challenge patents. That means fewer generics enter early, and prices stay higher longer. Canada and Australia have similar systems, but none match the U.S. for speed and volume of generic entry.
That’s why the Hatch-Waxman model has become a global reference. Countries looking to expand access to affordable medicines often look to the Orange Book and Paragraph IV as blueprints. But few have the legal infrastructure to support it.
What does ANDA stand for in the Hatch-Waxman Act?
ANDA stands for Abbreviated New Drug Application. It’s the streamlined application process created by the Hatch-Waxman Act that allows generic drug manufacturers to seek FDA approval without repeating expensive clinical trials. Instead, they must prove their product is bioequivalent to the brand-name drug already approved by the FDA.
Why is the Orange Book important for generic drugs?
The Orange Book lists all FDA-approved drugs and the patents associated with them. Generic manufacturers use it to know exactly which patents they must navigate before launching their product. If a patent isn’t listed, it can’t be used to block generic entry. It’s the official rulebook for when and how generics can enter the market.
What is a Paragraph IV certification?
A Paragraph IV certification is a legal statement made by a generic drug applicant that claims a patent listed in the Orange Book is either invalid or won’t be infringed by their product. This triggers a patent lawsuit from the brand-name company and, if the generic wins, grants them 180 days of exclusive market rights-making it the most valuable tool in the Hatch-Waxman system.
Does the Hatch-Waxman Act apply to biologics?
No. The Hatch-Waxman Act was designed for small-molecule drugs-pills and injections with simple chemical structures. Biologics, like insulin or monoclonal antibodies, are much more complex. Congress created a separate law in 2010 called the Biologics Price Competition and Innovation Act (BPCIA) to handle their approval. The pathways, requirements, and timelines are different.
How much money has the Hatch-Waxman Act saved the U.S. healthcare system?
According to the Congressional Budget Office, the Hatch-Waxman Act has saved the U.S. healthcare system approximately $1.7 trillion over the past decade. Generic drugs account for over 90% of prescriptions but only 23% of total drug spending, making them one of the biggest drivers of cost savings in American medicine.

