Anticoagulation Decision Tool
Patient Assessment
Managing blood thinners in patients with both kidney and liver disease isn’t just tricky-it’s one of the most high-stakes decisions in modern medicine. These patients aren’t just at higher risk for clots; they’re also far more likely to bleed dangerously. And the drugs we use to prevent clots? They don’t behave the same way in damaged organs. What works for a healthy 70-year-old with atrial fibrillation can kill someone with end-stage kidney failure or advanced cirrhosis.
Why Standard Rules Don’t Apply
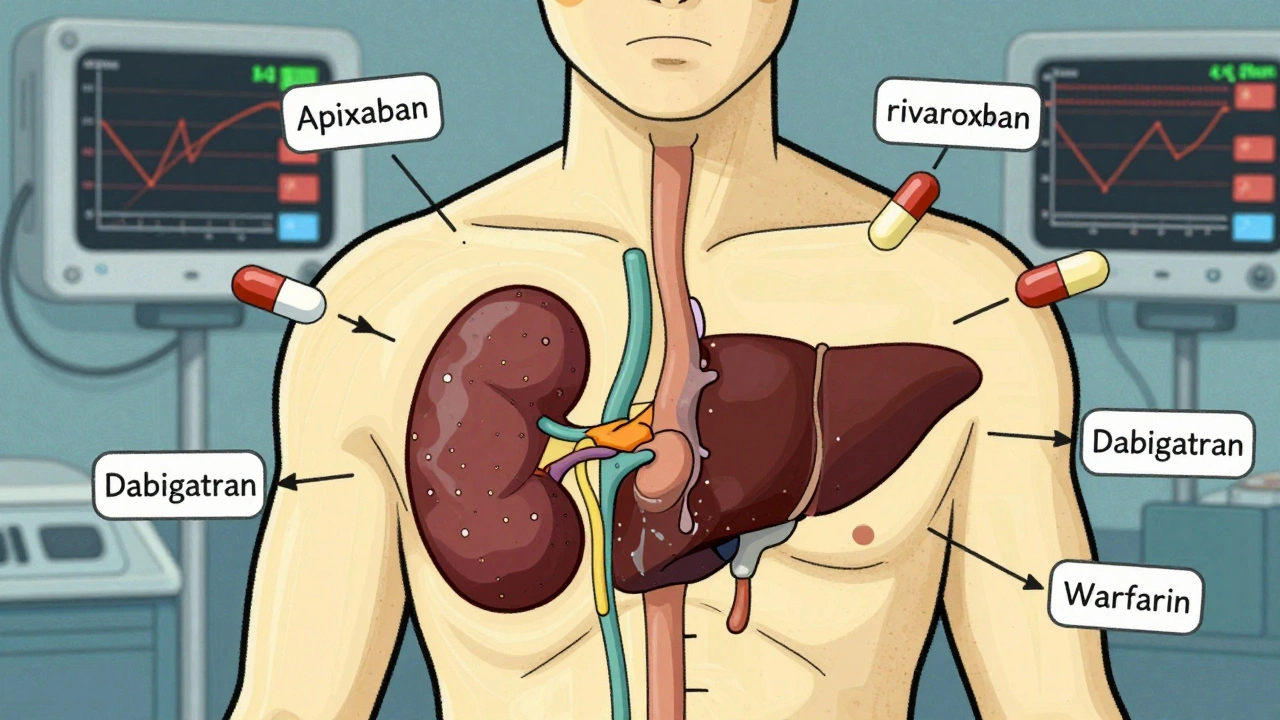
Most anticoagulant trials excluded people with severe kidney or liver disease. That means the labels on DOACs like apixaban, rivaroxaban, and dabigatran were built on data from people who didn’t have these conditions. When you look at the real world, the numbers tell a different story. About 24% of patients with atrial fibrillation also have chronic kidney disease, and 15% have liver disease. Many have both. These aren’t rare edge cases-they’re common, and they’re dangerous.The problem isn’t just about how the body processes the drug. It’s about how the disease changes the entire clotting system. In kidney failure, the body can’t clear the medication properly. In liver disease, the organ can’t make the proteins that help control clotting. You’re not just giving a drug to a sick person-you’re giving it to a body where the natural safety systems are broken.
Kidney Disease: Dose Adjustments Are Critical
Not all kidney disease is the same. The key is the eGFR, which measures how well your kidneys filter waste. For patients with stage 1-3a kidney disease (eGFR ≥45 mL/min), most DOACs can be used at standard doses. But once you hit stage 3b (eGFR 30-44 mL/min), you need to cut the dose. Apixaban drops from 5 mg twice daily to 2.5 mg. Rivaroxaban goes from 20 mg to 15 mg. Edoxaban drops from 60 mg to 30 mg. These aren’t guesses-they’re FDA-approved adjustments based on real pharmacokinetic data.Stage 4 and 5 kidney disease (eGFR under 30 mL/min) is where things get murky. The European Medicines Agency says don’t use rivaroxaban or apixaban here. The FDA says apixaban can still be used at 2.5 mg twice daily. Why the difference? Because the ARISTOTLE trial showed that in patients with eGFR below 30, apixaban cut major bleeding by 70% compared to warfarin. That’s not a small win. But it’s not a guarantee. In dialysis patients, apixaban levels drop to about 40% of normal. Rivaroxaban levels drop even more. So even if you give the same dose, the effect is weaker.
Warfarin isn’t a safe fallback. It’s harder to control. INR targets in advanced kidney disease often need to be lowered to 1.8-2.5 instead of the usual 2.0-3.0. And you have to check INR every two weeks, not once a month. Miss a test, and you’re either under-anticoagulated (risking stroke) or over-anticoagulated (risking brain bleed).
Liver Disease: The INR Lies
The liver makes clotting factors. It also makes anticoagulant proteins. In cirrhosis, both sides of the equation collapse. That’s why the INR-a number doctors rely on to measure warfarin’s effect-is meaningless in advanced liver disease. It only measures vitamin K-dependent factors. It ignores low platelets, poor fibrinogen production, and abnormal clot strength. A patient with a high INR might actually be at higher risk for clots than bleeding.The Child-Pugh score is the real guide here. Child-Pugh A (mild disease) can often handle standard DOAC doses. Child-Pugh B (moderate) needs caution-lower doses, closer monitoring. Child-Pugh C (severe) is a hard stop for DOACs. The RE-CIRRHOSIS study found these patients had more than five times the risk of major bleeding on DOACs compared to those with healthy livers.
Warfarin is still used here, but it’s a gamble. Only 45% of cirrhotic patients stay in the therapeutic range. That’s compared to 65% in people with normal livers. And when they do bleed? It’s often catastrophic. One study found 68% of hepatologists had seen at least one major bleed in the past year linked to anticoagulation in cirrhosis.

DOACs vs. Warfarin: The Real Numbers
When you strip away the theory, what do the numbers show?- In kidney disease, apixaban reduces major bleeding by 31% compared to warfarin in patients with eGFR between 25 and 30 mL/min.
- Dabigatran is cleared 80% by the kidneys. If your kidneys are failing, it builds up fast. That’s why it’s banned in eGFR under 30.
- Apixaban is cleared only 27% by the kidneys. That’s why it’s the only DOAC with any real data in dialysis patients.
- DOACs cut the risk of brain bleeds by 62% in kidney disease patients compared to warfarin.
- But in end-stage kidney disease with mechanical heart valves? Warfarin is still the only option. DOACs don’t work here.
For liver disease, DOACs reduce intracranial bleeding risk too-but only if the liver isn’t too damaged. In Child-Pugh C, even that benefit disappears.
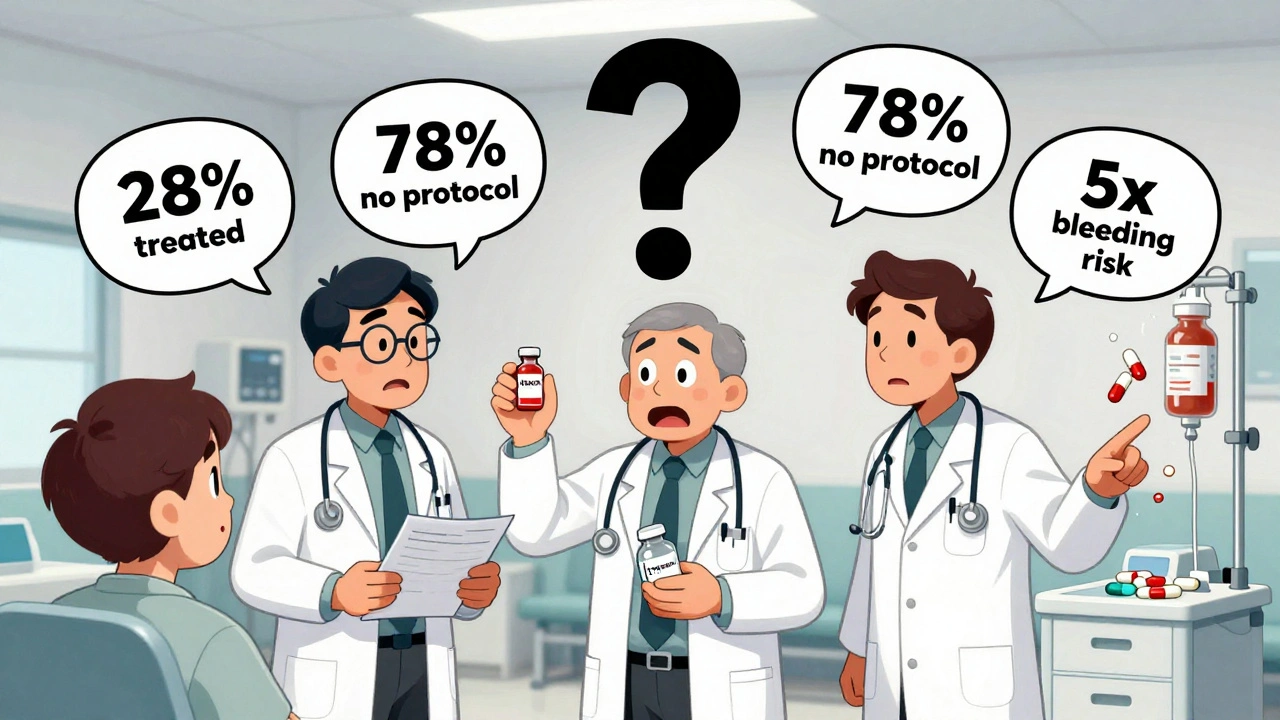
What Doctors Are Actually Doing
A 2021 registry of over 12,000 dialysis patients with atrial fibrillation found that only 28% were on any anticoagulant-even though 76% had a high stroke risk score. Of those who were treated, 63% got warfarin, 37% got a DOAC. Bleeding rates were lower with DOACs (14.2 per 100 patient-years vs. 18.7 with warfarin). But stroke rates? Nearly identical.On Reddit, nephrologists share horror stories and small wins. One doctor treated 15 dialysis patients on apixaban 2.5 mg daily for two years with zero bleeds. Another lost a patient to a retroperitoneal hemorrhage on the same dose. There’s no textbook answer. It’s risk assessment, experience, and sometimes, gut feeling.
In liver disease, hepatologists are starting to use TEG or ROTEM-tests that measure how well blood clots as a whole, not just one factor. But only 38% of U.S. hospitals have these tools. Most still rely on platelet counts and MELD scores. If platelets drop below 50,000/μL or MELD rises above 20, many stop anticoagulation entirely.
The Reversal Problem
If someone on a DOAC bleeds, can you reverse it? Yes-but it’s expensive and hard to get.- Andexanet alfa (Andexxa®) reverses apixaban and rivaroxaban. It costs $19,000 per dose. Only 45% of U.S. hospitals stock it.
- Idarucizumab (Praxbind®) reverses dabigatran. It’s cheaper at $3,500 per dose, but it’s useless for everyone else.
- Warfarin can be reversed with vitamin K and fresh frozen plasma. It’s slow, but it’s available everywhere.
And here’s the kicker: 78% of U.S. hospitals don’t have a formal protocol for managing anticoagulation in patients with both kidney and liver disease. That means decisions are made on the fly, by whoever’s on call. Mistakes happen. The Institute for Safe Medication Practices found these patients have over three times the rate of medication errors.
What’s Coming Next
Two major studies are underway. The MYD88 trial is randomizing 500 dialysis patients to either apixaban or warfarin, with results expected in 2025. The LIVER-DOAC registry is tracking 1,200 cirrhotic patients on DOACs across the world. These aren’t just academic exercises-they’ll change guidelines.The FDA is considering new labeling for apixaban in end-stage kidney disease based on modeling data. KDIGO, the global kidney health group, is updating its guidelines in late 2024, incorporating 17 new observational studies. That could mean more patients get treated safely.
For now, the message is simple: anticoagulation in kidney and liver disease isn’t about following a chart. It’s about understanding the patient-their organs, their risks, their life. There’s no perfect drug. No perfect dose. Just better choices, made with more data, more caution, and more teamwork.
Can DOACs be used in patients on dialysis?
Apixaban is the only DOAC with any real-world data in dialysis patients. Most guidelines recommend 2.5 mg twice daily based on pharmacokinetic studies and subgroup analyses from the ARISTOTLE trial. Rivaroxaban and edoxaban are not recommended due to higher bleeding risk and lack of safety data. Dabigatran is contraindicated because it’s cleared mostly by the kidneys. Warfarin remains an option, but requires frequent INR checks and carries a higher bleeding risk.
Is INR reliable in liver disease?
No. INR only measures vitamin K-dependent clotting factors, which are low in liver disease. But in cirrhosis, patients also have low platelets, low fibrinogen, and poor clot quality. A high INR doesn’t mean they’re at high bleeding risk-it might mean they’re at high clotting risk. Tools like TEG or ROTEM give a fuller picture but are only available in about 38% of U.S. hospitals. Most doctors rely on platelet count and MELD score instead.
Which anticoagulant is safest for kidney disease?
Apixaban is the safest DOAC for kidney disease, especially in stages 3b-4. It’s cleared least by the kidneys (only 27%), and studies show it reduces major bleeding by 31% compared to warfarin in patients with eGFR between 25 and 30 mL/min. Rivaroxaban and edoxaban are less safe in advanced disease. Dabigatran should be avoided if eGFR is under 30. For dialysis patients, apixaban 2.5 mg twice daily is the only DOAC with any consistent safety data.
Can you use DOACs in Child-Pugh C cirrhosis?
No. DOACs are contraindicated in Child-Pugh C cirrhosis. These patients have a 5.2-fold higher risk of major bleeding compared to those with healthy livers. The liver can’t make enough clotting factors or clear drugs properly. Warfarin is still used in some cases, but it’s unpredictable and hard to manage. The safest approach is often to avoid anticoagulation unless the risk of clotting (like portal vein thrombosis) is very high and outweighs the bleeding risk.
What should you do if a patient with liver disease needs anticoagulation?
Start by assessing the liver function using Child-Pugh score and MELD score. If it’s Child-Pugh A, consider a DOAC at standard dose. For Child-Pugh B, reduce the DOAC dose or use warfarin with frequent monitoring. For Child-Pugh C, avoid DOACs entirely. Check platelet count monthly-if it drops below 50,000/μL, stop anticoagulation. Consider TEG or ROTEM if available. Always involve hepatology and hematology. Never rely on INR alone.

Comments (10)
Richard Eite
December 7, 2025 AT 13:42Apixaban is the only thing that works in dialysis and everyone knows it
Katherine Chan
December 8, 2025 AT 11:08Finally someone is talking sense about this. So many patients get ignored because the rules dont fit them
Appreciate the real world data
Nikhil Pattni
December 8, 2025 AT 17:01Look Ive been doing this for 18 years and I can tell you DOACs are a trap in liver disease no matter what the papers say
My buddy in Houston lost a guy last month on apixaban 2.5mg even though he was Child-Pugh B
INR was 1.9 and he bled out in 4 hours
And dont get me started on how hospitals dont even have reversal agents
Andexxa costs more than my car and half the ERs dont stock it
Warfarin is messy but at least you can fix it with FFP and vitamin K
Plus the FDA and KDIGO are just playing politics with guidelines
They dont live in the trenches where patients bleed out because some algorithm said it was safe
And dont even get me started on how nephrologists dont talk to hepatologists
Its a disaster waiting to happen and everyone just nods and writes the script
Its not medicine its a gamble with a $19k dice roll
om guru
December 10, 2025 AT 13:57Apixaban remains the most rational choice in advanced renal impairment when anticoagulation is indicated
Pharmacokinetic data supports its use even in dialysis patients
Outcome studies demonstrate lower bleeding risk compared to warfarin
Guidelines must be interpreted with clinical context
Individual patient factors outweigh algorithmic recommendations
Team based decision making is essential
Do not rely solely on eGFR or INR
Consider comorbidities and bleeding history
Document rationale thoroughly
Continual monitoring is non negotiable
Therapeutic success depends on vigilance not convenience
Resist the temptation to avoid anticoagulation due to fear
Some patients will benefit significantly
Do not let institutional limitations dictate care
Advocate for access to reversal agents when possible
Sarah Gray
December 12, 2025 AT 10:38Apixaban is not cleared 27% by the kidneys it's renally excreted to the tune of 25% with 75% hepatic metabolism
And the ARISTOTLE subgroup analysis was not powered for dialysis patients
Also Child-Pugh C is not a contraindication it's a relative one
And you're forgetting that MELD score correlates with coagulopathy better than Child-Pugh
And TEG is not available in 38% of US hospitals it's available in under 15%
And the RE-CIRRHOSIS study had selection bias
And the FDA hasn't approved any new labeling for apixaban in ESKD yet
And you're misrepresenting the 2021 registry data
And you're conflating observational data with RCT evidence
And you're ignoring the fact that DOACs are still off label in most of these scenarios
And you're not addressing the lack of prospective data
And you're using anecdotal Reddit stories as clinical evidence
And you're not mentioning the cost burden on patients
And you're omitting that warfarin has better long term safety data in cirrhosis
And you're not discussing the impact of proteinuria on DOAC clearance
And you're not considering the role of albumin binding
And you're not addressing the potential for drug interactions with diuretics and antibiotics
And you're not acknowledging that nephrologists and hepatologists rarely communicate
And you're not discussing the ethical implications of treating patients with no clear evidence base
And you're not mentioning that the MYD88 trial results are still 18 months away
And you're ignoring the fact that most patients with both CKD and cirrhosis are excluded from all trials
And you're not addressing the fact that dialysis membranes vary in DOAC clearance
And you're not considering the impact of ascites on pharmacokinetics
And you're not discussing the role of platelet transfusion in bleeding risk
And you're not acknowledging that INR is still the most accessible and widely understood metric
And you're not addressing the fact that reversal agents are rarely used in practice due to cost and access
And you're not mentioning that 78% of hospitals lack protocols because they're not evidence based
And you're not considering the psychological burden on providers who are forced to make decisions without data
And you're not acknowledging that some patients refuse anticoagulation entirely due to fear
And you're not discussing the role of shared decision making
And you're not addressing the fact that DOACs are not approved for mechanical valves
And you're not mentioning that apixaban 2.5mg twice daily is not FDA approved for dialysis
And you're not acknowledging that the 70% bleeding reduction in ARISTOTLE was for all comers not just dialysis
And you're not discussing the potential for underdosing leading to stroke
And you're not considering the impact of malnutrition on clotting factor synthesis
And you're not addressing the fact that many patients on dialysis have atrial fibrillation secondary to uremia not embolic risk
And you're not mentioning that the 28% anticoagulation rate in the registry is actually higher than expected
And you're not acknowledging that the 14.2 vs 18.7 bleeding rate is not statistically significant in some analyses
And you're not discussing the role of frailty and life expectancy
And you're not addressing the fact that most patients with both CKD and cirrhosis die of other causes before stroke or bleed occurs
And you're not considering the impact of socioeconomic status on medication adherence
And you're not acknowledging that the real problem is lack of research not lack of guidelines
And you're not mentioning that the only thing worse than an incorrect anticoagulation decision is no decision at all
And you're not discussing the ethical obligation to treat despite uncertainty
And you're not addressing the fact that guidelines are meant to guide not dictate
And you're not acknowledging that the word contraindicated is often misused in clinical practice
And you're not considering the role of palliative care in these complex patients
And you're not mentioning that the goal is not to eliminate risk but to minimize it
And you're not acknowledging that the best anticoagulation strategy is often no anticoagulation at all
And you're not addressing the fact that most patients don't have access to hepatology or nephrology specialists
And you're not discussing the role of primary care in managing these patients
And you're not mentioning that the majority of bleeding events occur in the first 30 days
And you're not considering the impact of polypharmacy on drug interactions
And you're not acknowledging that the only randomized trial in this population is still ongoing
And you're not addressing the fact that the data you're citing is from 2021 and new evidence is emerging
And you're not mentioning that the MYD88 trial will answer most of these questions
And you're not acknowledging that the current standard of care is a compromise
And you're not discussing the role of patient preferences in decision making
And you're not addressing the fact that some patients prefer warfarin because they understand it
And you're not considering the impact of cultural beliefs on treatment adherence
And you're not mentioning that the real issue is systemic underinvestment in complex patient care
And you're not acknowledging that the problem isn't the drugs it's the system
And you're not addressing the fact that we're treating patients with data from people who aren't like them
And you're not mentioning that the only thing worse than a bad decision is a decision made without thinking
And you're not acknowledging that every patient is different
And you're not discussing the role of clinical judgment
And you're not addressing the fact that medicine is not a science it's an art
And you're not mentioning that the goal is not to follow the guidelines but to care for the person
And you're not acknowledging that the most dangerous thing in medicine is certainty
Darcie Streeter-Oxland
December 12, 2025 AT 18:21The notion that apixaban is safe in end-stage renal disease remains empirically unsupported by high quality evidence
The ARISTOTLE subgroup analysis was underpowered and post hoc
The FDA's allowance of 2.5 mg twice daily is based on pharmacokinetic modeling not clinical outcomes
There is no prospective randomized trial demonstrating net clinical benefit in dialysis patients
Warfarin remains the only anticoagulant with longitudinal safety data in this population
The 70% reduction in bleeding cited is misleading as it compares apixaban to warfarin in a mixed cohort not dialysis alone
INR remains the most accessible and standardized tool despite its limitations
TEG and ROTEM are not standard of care and remain research tools in most institutions
The cost of reversal agents is prohibitive and their availability is inconsistent
Guidelines must be interpreted with caution in the absence of level 1 evidence
Anticoagulation in complex multisystem disease requires multidisciplinary consensus
It is premature to claim apixaban as the preferred agent without definitive trial data
The current practice pattern reflects therapeutic nihilism disguised as innovation
More research is needed before changing established standards
The burden of proof lies with proponents of DOACs in this population
Until then caution is the only ethical course
Chris Marel
December 13, 2025 AT 09:10Thanks for laying this out so clearly
I've had patients where we just stopped everything because no one knew what to do
It's scary how much we're guessing
Appreciate the honesty about how messy it is
Hope the MYD88 trial gives us better answers soon
Haley P Law
December 14, 2025 AT 04:15So apixaban is the only thing that works in dialysis and the system is still broken
And no one has reversal agents
And doctors are flying blind
And patients are dying
And the FDA is dragging their feet
And we're all just waiting for a trial that won't come for another two years
WHY IS THIS STILL HAPPENING
WE KNOW THIS
ian septian
December 15, 2025 AT 06:16Apixaban 2.5 mg BID in dialysis is the best option we have
Don't overthink it
Just do it right
Brianna Black
December 15, 2025 AT 10:10What strikes me most is not the pharmacology but the human cost
Patients with end-stage kidney and liver disease are caught between two systems that rarely speak to each other
They are treated by specialists who see only one organ
But their bodies are screaming as one
And the guidelines are written for healthy populations
And the reversal agents are locked in vaults because they're too expensive
And the nurses are overworked
And the pharmacists are overwhelmed
And the patients are terrified
And the families are confused
And the doctors are exhausted
This is not a clinical problem
This is a moral failure
Our medical system is designed for efficiency not compassion
And we are failing our most vulnerable
Not because we lack knowledge
But because we lack the will to change
Until we treat the whole person not just the lab values
Until we fund research for the rare not the profitable
Until we make reversal agents accessible to every hospital
Until we train providers to communicate across specialties
Until we listen to the nurses and the social workers and the patients themselves
We will keep having these tragedies
And no algorithm will ever fix that