Many people don’t realize that the pills they take for everyday problems-headaches, allergies, depression, or joint pain-could be quietly raising their blood pressure. It’s not just about aging or diet. Sometimes, the culprit is something you’re taking on purpose. Medication-induced hypertension affects millions, yet it’s often missed because it doesn’t come with obvious symptoms. If your blood pressure suddenly spikes after starting a new drug, or if your numbers won’t budge despite treatment, the cause might be hiding in your medicine cabinet.
What Medications Can Raise Your Blood Pressure?
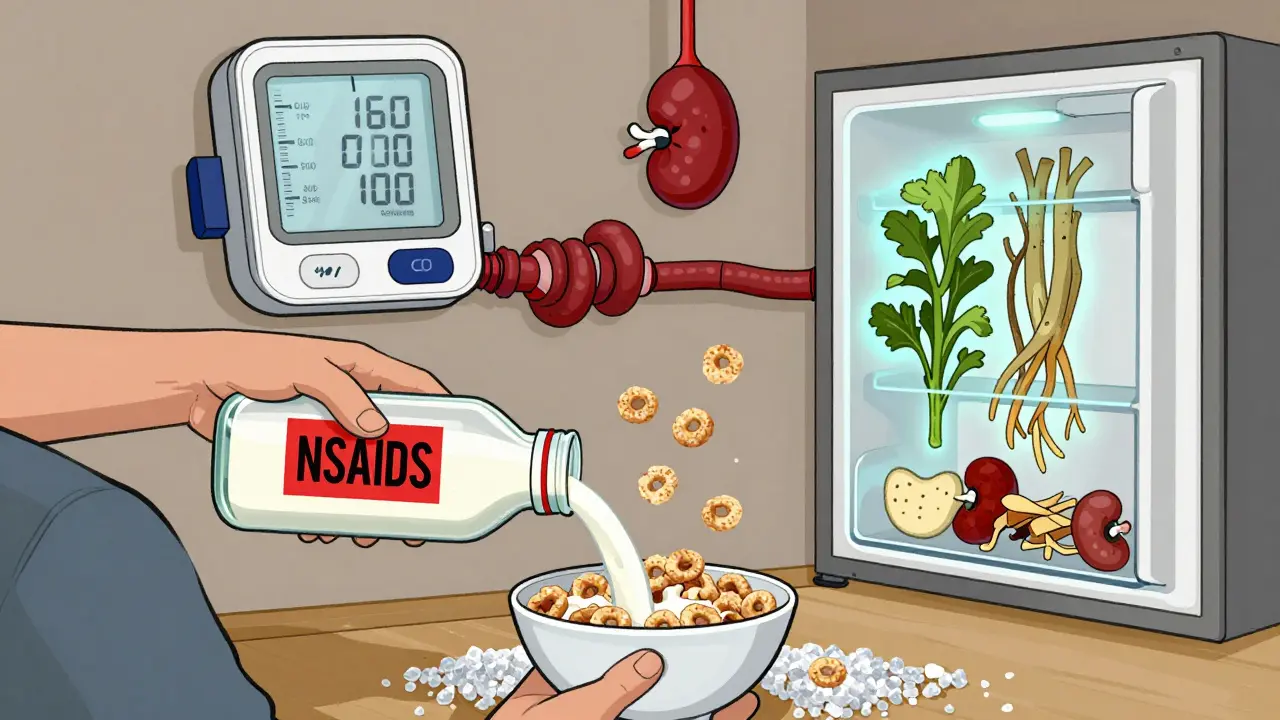
Over 50 common medications are linked to elevated blood pressure. Some are prescription, others are sold over the counter. The biggest offenders include:
- NSAIDs like ibuprofen (Advil, Motrin) and naproxen (Aleve): These painkillers reduce kidney function slightly, causing fluid retention. In people with existing high blood pressure, ibuprofen can raise systolic pressure by 5-10 mm Hg within two weeks.
- Corticosteroids like prednisone: Used for inflammation, autoimmune diseases, or asthma, these drugs mimic cortisol and cause sodium and water buildup. At doses above 20 mg/day for more than four weeks, up to 60% of users develop high blood pressure.
- Antidepressants such as venlafaxine (Effexor): These increase norepinephrine levels, tightening blood vessels. Doses above 150 mg/day raise BP in 8-15% of patients.
- Decongestants like pseudoephedrine and phenylephrine: Found in cold and sinus meds, they constrict blood vessels within hours. A single dose can spike systolic pressure by 5-10 mm Hg.
- ADHD stimulants like Adderall and Ritalin: These activate the nervous system. Dextroamphetamine raises BP in nearly 25% of users.
- Erythropoietin (Procrit): Used for anemia, especially in kidney disease patients, it thickens the blood and increases resistance in vessels.
- HIV medications (HAART): Especially in older adults, these can cause delayed BP increases after six months of use.
Even herbal supplements like St. John’s Wort and licorice root can interfere with blood pressure control. Many patients aren’t warned about these risks because they assume OTC means safe.
How These Drugs Actually Raise Blood Pressure
Each class works differently, but they all push blood pressure up through one of three main pathways:
- Sodium and water retention: NSAIDs and corticosteroids block the kidneys’ ability to flush out salt. This increases blood volume, forcing the heart to pump harder.
- Vasoconstriction: Decongestants and some antidepressants trigger receptors that tighten arteries. This raises resistance, making it harder for blood to flow.
- Increased sympathetic activity: Stimulants and SNRIs overactivate the fight-or-flight system, speeding up heart rate and constricting vessels.
For example, ibuprofen reduces blood flow to the kidneys by 15-20% within two hours. Prednisone at 30 mg/day can increase plasma volume by 10% in just three days. Pseudoephedrine raises vascular resistance by 25-30% within an hour. These aren’t minor changes-they’re measurable, dangerous shifts.
How to Monitor for Drug-Induced Hypertension
Waiting for symptoms like headaches or dizziness is too late. High blood pressure often has none. Here’s how to catch it early:
- Take a baseline reading before starting any new medication. Write it down.
- Check your BP at 1-2 weeks after starting the drug. Then again at 4-6 weeks.
- Use home monitoring: Take two readings in the morning and two in the evening for seven days after starting or changing a dose. Average the last six days’ readings.
- For high-risk patients (those with existing hypertension, kidney disease, or on multiple BP-raising drugs), ask your doctor about ambulatory blood pressure monitoring (ABPM). This tracks your pressure over 24 hours and catches spikes you might miss at the clinic.
- If you’re on steroids: Check your BP daily for the first month. Watch for orthostatic changes-when your reading drops significantly when you stand up. That’s a sign your body is struggling to adjust.
Many patients don’t realize their BP is rising because they only check it during doctor visits. A 2023 study found that 68% of people on NSAIDs who developed high blood pressure had no idea until they had a hypertensive episode.
What to Do If a Medication Is Raising Your BP
Don’t stop any medication without talking to your doctor. But here’s what you can do:
- Try switching: For pain, swap ibuprofen for acetaminophen (up to 3,000 mg/day) or celecoxib. Celecoxib raises BP by only 2.4 mm Hg on average, compared to 5.7 mm Hg for ibuprofen.
- Use non-decongestant options: For sinus relief, try saline sprays, humidifiers, or antihistamines like loratadine (Claritin) instead of pseudoephedrine.
- Adjust antidepressants: If venlafaxine is raising your BP, your doctor might switch you to an SSRI like sertraline, which has less effect on blood pressure.
- Reduce the dose: Sometimes lowering the steroid dose or spacing out stimulant doses helps. Not always possible, but worth discussing.
If you can’t stop the medication-like if you need prednisone for lupus or Adderall for ADHD-your doctor may add an antihypertensive. Calcium channel blockers (like amlodipine) and thiazide diuretics (like hydrochlorothiazide) work best. Beta-blockers? They’re not ideal. Studies show they only help 45% of the time, compared to 72% for calcium channel blockers, because they don’t reverse vasoconstriction.
Lifestyle Changes That Help
Even if you can’t stop the medication, small changes make a big difference:
- Limit sodium to under 1,500 mg per day. That’s less than one teaspoon of salt. Avoid processed foods, canned soups, and restaurant meals.
- Get more potassium: Aim for 2,500-3,500 mg daily from bananas, spinach, sweet potatoes, beans, and yogurt. Potassium helps your body flush out sodium.
- Move for 150 minutes a week: Brisk walking, cycling, or swimming lowers BP by 5-8 mm Hg in drug-induced cases.
- Limit alcohol and quit smoking: Both worsen the effects of BP-raising drugs.
A 2023 meta-analysis showed that combining these changes with medication adjustments cut systolic pressure by an average of 10 mm Hg in patients with drug-induced hypertension.

Why This Is Often Overlooked
Doctors don’t always ask about OTC meds. A 2023 European study found only 22% of primary care providers routinely check if their hypertensive patients are taking NSAIDs or decongestants. Patients don’t think to mention them either. On Reddit’s hypertension forum, hundreds of people shared stories of being told their high BP was just “stress” or “aging,” only to find out later that their daily Advil was the cause.
One patient in Birmingham reported her BP stayed at 160/100 for months. Her doctor kept increasing her meds. Then she mentioned she’d been taking Sudafed every winter for her sinuses. Switching to a non-decongestant version brought her BP down to 120/80 in three weeks.
Another took St. John’s Wort for low mood. She didn’t think it counted as a “real” drug. It spiked her BP so high she ended up in the ER. She wasn’t warned. No one asked.
What You Can Do Right Now
Here’s a simple checklist:
- Make a full list of everything you take: prescriptions, OTC, vitamins, herbs, supplements.
- Check if any are on the high-risk list above.
- Review your latest BP readings. Did they start rising after you began a new drug?
- Ask your doctor: “Could any of my medications be raising my blood pressure?”
- Start home monitoring if you haven’t already.
If you’re on long-term steroids, NSAIDs, or antidepressants, schedule a BP review every three months-even if you feel fine. Don’t wait for symptoms.
What’s Changing in 2026
Things are improving. The FDA now requires stronger warnings on NSAID labels. The American Heart Association launched a free online calculator that helps doctors estimate BP risk based on your meds. Pharmacist-led medication reviews are being tested in clinics across the U.S., and early results show a 28% drop in uncontrolled hypertension among patients who get them.
By 2030, experts predict a 15-20% reduction in complications from medication-induced hypertension thanks to better screening and awareness. But that won’t happen unless patients speak up and doctors ask the right questions.
Can over-the-counter painkillers really raise blood pressure?
Yes. NSAIDs like ibuprofen and naproxen are among the most common causes of medication-induced hypertension. Ibuprofen can raise systolic blood pressure by 5-10 mm Hg in people with existing high blood pressure, and even healthy individuals can see a 3-5 mm Hg increase after two weeks of regular use. Naproxen has a milder effect, but neither is truly safe for long-term use if you have hypertension.
How long does it take for blood pressure to return to normal after stopping the medication?
It depends on the drug. For NSAIDs and decongestants, BP often drops within 2-4 weeks after stopping. For corticosteroids, it can take 4-8 weeks, especially after long-term use. Antidepressants and stimulants may take 1-3 weeks. Always monitor your BP during this time and don’t stop medication abruptly without medical advice.
Are herbal supplements safe for people with high blood pressure?
No, not all are. St. John’s Wort, licorice root, ginseng, and ephedra can all raise blood pressure or interfere with blood pressure medications. Many people assume herbal means safe, but these substances can cause dangerous spikes. Always tell your doctor what supplements you’re taking.
Why aren’t doctors more aware of this issue?
Many physicians focus on prescribing for the main condition-pain, depression, allergies-and don’t routinely screen for BP side effects. Studies show only 58% of doctors can correctly identify all high-risk medications. Patient surveys also reveal that most people aren’t warned about these risks when they pick up an OTC bottle. It’s a systemic gap, not just individual negligence.
Should I stop taking my medication if my blood pressure goes up?
Never stop a prescribed medication on your own. Some drugs, like steroids or antidepressants, can cause serious withdrawal effects if stopped suddenly. Instead, contact your doctor. They can help you adjust the dose, switch to a safer alternative, or add a blood pressure medication that works with your current treatment.
Is it safe to take ibuprofen if I have high blood pressure?
It’s not recommended. Ibuprofen can worsen hypertension and reduce the effectiveness of your blood pressure medications. If you need pain relief, ask your doctor about acetaminophen or celecoxib, which have less impact on blood pressure. Even occasional use can be risky if you’re already on antihypertensives.


Comments (12)
Michael Burgess
January 1, 2026 AT 14:17Just got back from my doc and realized I’ve been taking ibuprofen daily for my back pain. My BP was 158/96 last week. I switched to acetaminophen yesterday and already feel lighter. Home monitor says 132/84 this morning. Who knew? OTC doesn’t mean harmless. Thanks for the post - this is the kind of info that saves lives.
Angela Fisher
January 3, 2026 AT 05:49THEY KNOW. THEY ALL KNOW. The pharmaceutical companies? They’ve been hiding this for decades. NSAIDs? Steroids? Even your ‘natural’ supplements? It’s all a money game. Your doctor won’t tell you because they’re paid by Big Pharma. I saw a whistleblower video - they literally train med students to ignore drug-induced hypertension. That’s why your BP won’t drop. They don’t want you to stop the pills. They want you on MORE pills. Wake up.
Palesa Makuru
January 4, 2026 AT 21:47Wow. So you're telling me my daily Sudafed for sinusitis is quietly turning me into a walking hypertensive? I mean, I’ve been taking it since college. I thought it was just ‘part of being a grown-up.’ Now I feel like a lab rat in a corporate experiment. Do you think my insurance will cover the therapy I need after this revelation?
Neela Sharma
January 5, 2026 AT 22:22My aunt in Delhi took licorice root for ‘digestion’ - BP hit 190/110. ER. ICU. Three days. She didn’t even know it was a drug. We all think ‘herbal’ = safe. But nature doesn’t care if you’re diabetic or hypertensive. It just reacts. Listen to your body. Not the bottle.
Shruti Badhwar
January 7, 2026 AT 07:21While the data presented is compelling, it's important to contextualize risk. Not every patient on NSAIDs develops hypertension, and individual variability in pharmacokinetics plays a significant role. The meta-analysis cited suggests a population-level trend, but clinical decision-making requires personalized assessment. I recommend discussing biomarkers like urinary sodium-to-potassium ratios alongside BP monitoring for more accurate risk stratification.
Haley Parizo
January 8, 2026 AT 21:19It’s not just about meds. It’s about how we’ve outsourced our health to pills. We treat symptoms like bugs to be sprayed, not signals to be heard. Your body isn’t broken - it’s begging you to listen. NSAIDs? Maybe your inflammation is screaming for sleep, for stress reduction, for real food. Steroids? Maybe your immune system is drowning in processed sugar. We’ve forgotten that healing isn’t a prescription - it’s a conversation. And we’ve been talking over it with chemicals.
Brittany Wallace
January 9, 2026 AT 06:48Thank you for this. I’ve been on Effexor for 5 years and never knew it could do this. My BP was always ‘fine’ at the clinic - until I started home monitoring. Now I’m working with my doctor to switch to sertraline. It’s scary to change meds, but safer than ignoring it. 🙏
Hank Pannell
January 9, 2026 AT 14:44Interesting how the FDA’s new labeling requirements are a band-aid. The real issue? The medical-industrial complex treats hypertension as a disease to be managed, not a symptom to be investigated. We’re not asking: Why is this person on 5 BP meds? Why did they start taking prednisone? Who’s tracking polypharmacy? We’re just adding more pills to fix the last pill’s side effect. It’s pharmacological whack-a-mole. We need systems-level change - not just patient checklists.
Wren Hamley
January 10, 2026 AT 23:19My dad’s on Adderall for ADHD. His BP went from 120/80 to 150/95 in 3 months. He thought it was ‘just stress.’ We switched to non-stimulant meds and he’s down to 128/82. No more jitters, no more spikes. Doctors need to screen for stimulants like they do for smoking. It’s not ‘just ADHD’ - it’s cardiovascular risk.
Liam Tanner
January 11, 2026 AT 08:55Just wanted to add - if you’re on long-term steroids, don’t forget to check your potassium. Prednisone drains it like a sieve. Low K+ makes BP harder to control, even if you’re on diuretics. I started eating bananas and spinach daily - my BP dropped 8 points without changing meds. Small wins matter.
Sarah Little
January 12, 2026 AT 15:05St. John’s Wort + my beta-blocker = ER visit. The pharmacist didn’t warn me. The doctor didn’t ask. I thought ‘natural’ meant ‘no interactions.’ Turns out, it’s a CYP3A4 nightmare. I’m now on an SSRI and monitoring daily. If you’re on any med, even ‘harmless’ herbs - get a med review. Seriously. It’s not paranoia. It’s survival.
Ian Detrick
January 13, 2026 AT 04:21My favorite part? The 2026 FDA changes. Change is possible. We’ve been told for years that hypertension is ‘lifestyle’ or ‘genetics’ - but this? This is preventable. We just need to start asking the right questions. Not just ‘Are you taking anything?’ but ‘What are you taking every day - even if you think it’s nothing?’ That’s the shift. And it starts with us.