When the temperature climbs, most people think about drinking more water, staying in the shade, and wearing light clothes. But for people taking diuretics or anticholinergics, heat isn’t just uncomfortable-it can be life-threatening. These medications, commonly prescribed for high blood pressure, heart failure, overactive bladder, and depression, interfere with the body’s natural ability to cool down. And many people don’t even realize they’re at risk.
How Diuretics Put You at Risk in the Heat
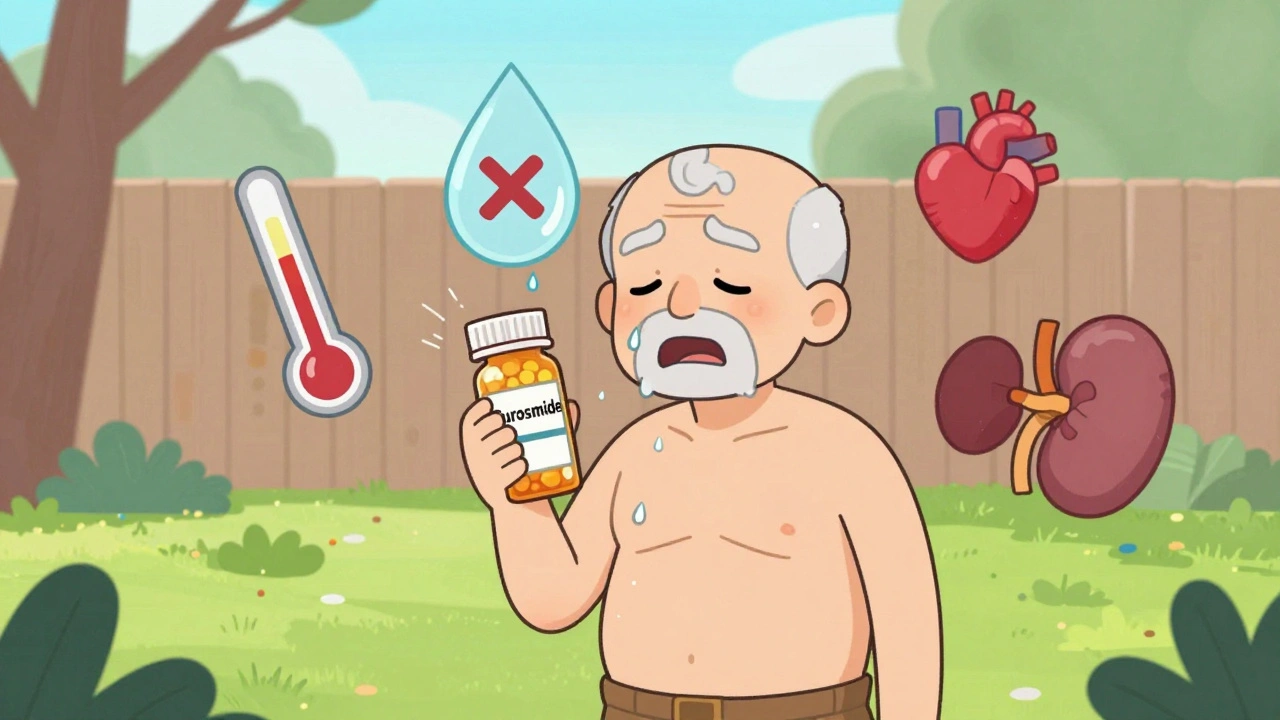
Diuretics-often called water pills-work by making your kidneys flush out extra salt and water. That’s great for lowering blood pressure or reducing swelling. But in hot weather, that same mechanism becomes dangerous. When you sweat, you lose fluid. Diuretics make you lose even more. The result? Your blood volume drops, your heart has to work harder, and your body can’t cool itself properly.
Common diuretics like furosemide (Lasix), hydrochlorothiazide (Microzide), and chlorthalidone (Hygroton) are taken by over 32 million Americans. A 2022 study of 1.2 million Medicare beneficiaries found that people on loop diuretics had a 37% higher chance of being hospitalized for heat-related illness-even when temperatures were only around 80°F (26.7°C). That’s not a heatwave. That’s a normal summer day.
It’s not just about dehydration. Diuretics also flush out potassium, magnesium, and sodium. Low potassium can cause muscle cramps, irregular heartbeat, and weakness. In extreme heat, that puts extra strain on your heart. Dr. Myrna Alexander Nickens from the University of Mississippi Medical Center puts it simply: “Diuretics are very effective in lowering blood pressure. But diuretics can dehydrate you.” And that dehydration happens faster than you think.
Why Anticholinergics Are Even More Dangerous
If diuretics cut your body’s water supply, anticholinergics shut off your cooling system entirely. These drugs block acetylcholine, a chemical that tells your sweat glands to activate. No sweat. No cooling. No warning.
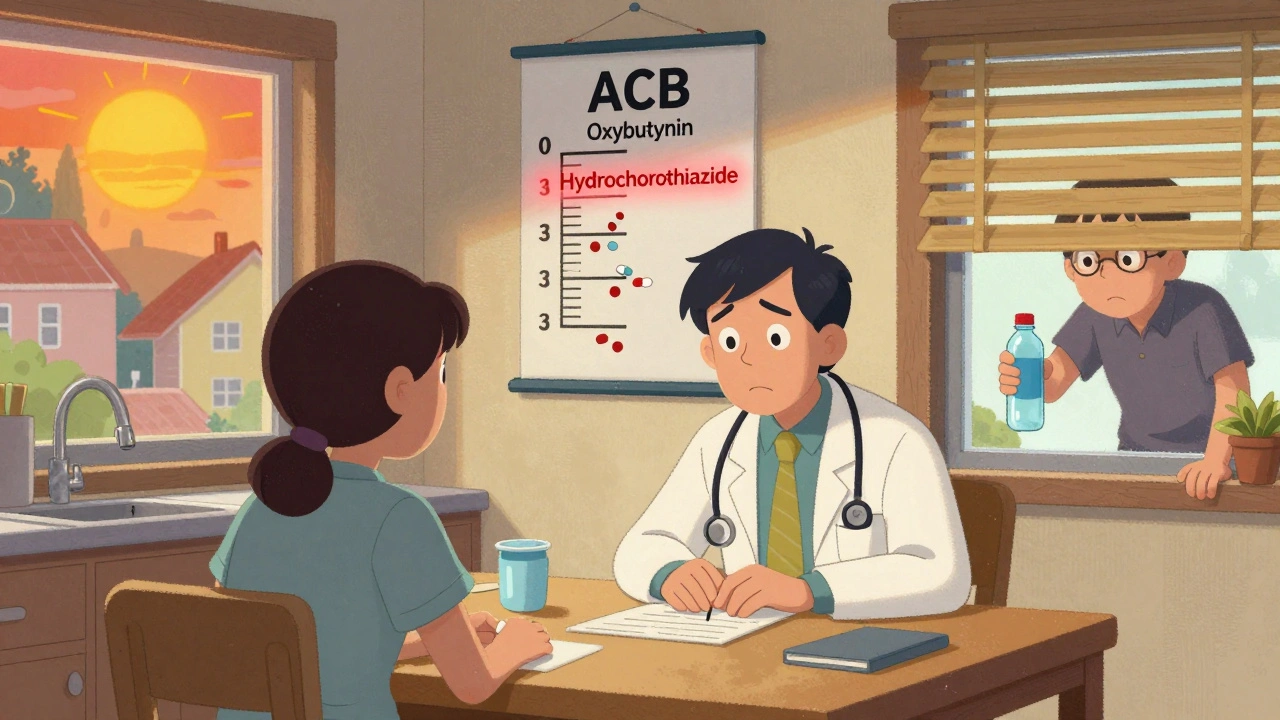
Medications like oxybutynin (Ditropan), tolterodine (Detrol), and amitriptyline (Elavil) are often prescribed for overactive bladder, Parkinson’s, depression, or chronic pain. But they carry a high anticholinergic burden score (ACB = 3), meaning they strongly suppress sweating. Studies show these drugs can reduce sweat production by 30% to 50%. That’s like turning off your body’s air conditioner.
What’s worse? Anticholinergics can cause confusion, dizziness, and memory problems-symptoms that look a lot like early heat illness. So you might not realize you’re overheating until it’s too late. During the 2021 Pacific Northwest heat dome, 63% of the people who died from heat exposure were taking either a diuretic or an anticholinergic. Many of them didn’t feel thirsty. They didn’t feel hot. They just got confused… and then collapsed.
What Happens When Both Medications Are Taken Together
It’s not just one drug. Many older adults take multiple medications. A person with heart failure might be on a diuretic, a beta-blocker, and an anticholinergic for bladder control. Each one chips away at their ability to handle heat. The CDC warns that these combinations can have a “compounding effect,” where the risks aren’t just added-they multiply.
Imagine someone on hydrochlorothiazide (losing fluid) and oxybutynin (not sweating). Their body can’t hold onto water, and it can’t release heat. Their core temperature rises. Their heart races. Their brain gets foggy. By the time they call for help, it’s often too late. Research from the Journal of Thermal Biology shows that even healthy young men under controlled heat stress show dangerous temperature spikes when on high-ACB drugs. For older adults with chronic illness, the risk is far worse.

What You Should Do: Practical Heat Safety Steps
Don’t stop your meds. That’s the first rule. But you do need to adjust how you live in hot weather.
- Drink water-even if you’re not thirsty. Your body won’t signal you properly. Set a timer to drink 8 ounces every hour if you’re outside or in a hot room. Don’t wait until your mouth feels dry.
- Check your fluid restrictions. If you have heart failure and your doctor told you to limit fluids, ask if that still applies during heatwaves. The CDC says fluid restrictions may need to be temporarily relaxed. Don’t guess-call your provider.
- Wear the right clothes. Light-colored, loose cotton lets air move and helps evaporate sweat-even if you’re sweating less. Avoid dark colors and synthetic fabrics like polyester.
- Use sunscreen. Many anticholinergics make your skin more sensitive to the sun. SPF 30+ is a must. Sunburn makes it harder for your body to cool down.
- Stay indoors during peak heat. 10 a.m. to 4 p.m. is the danger zone. Use fans, close blinds, and if you have AC, use it-even if you think it’s “too expensive.” Heat kills faster than electricity bills.
- Know the warning signs. Dizziness, headache, nausea, confusion, rapid heartbeat, dry skin (yes, dry skin is a red flag), and muscle cramps aren’t just “feeling off.” They’re signs your body is failing. Call 999 or go to A&E if you or someone you care about has these symptoms.
Ask Your Doctor: The Critical Questions to Ask
Don’t wait for a heatwave to think about this. Talk to your doctor now.
- “Is my medication known to increase heat risk?”
- “What’s my anticholinergic burden score?” (Ask for the ACB score-some drugs are worse than others.)
- “Should I adjust my dose during summer months?”
- “Do I need a buddy system? Can someone check on me daily when it’s hot?”
- “What symptoms mean I need to go to the hospital right away?”
At Massachusetts General Hospital, 42% of heart failure patients on diuretics needed temporary dose changes during the 2022 heatwave. That’s not rare. That’s expected. But most patients never discussed it with their doctor.
Why This Isn’t Just “Common Sense”
There’s a myth that if you’re careful, you’ll be fine. But heat illness doesn’t wait for common sense. It sneaks up. People think, “I’ve been fine before,” or “I don’t feel that hot.” But your body isn’t signaling right. Your brain isn’t working right. And your meds are silently sabotaging your survival system.
Studies show that even moderate heat-below official heatwave thresholds-can be deadly for people on these drugs. And the problem is getting worse. Between 1970 and 2020, the number of days over 90°F (32.2°C) in the U.S. jumped by 47%. The UK is seeing the same trend. Birmingham’s hottest summers are now hotter than ever.
The CDC, Johns Hopkins, and the EPA all agree: we’re not doing enough. Most research on medication-heat risks comes from small studies or young, healthy men. We don’t have enough data on older women with kidney disease, or people with dementia on multiple anticholinergics. But we have enough to know this: if you take these drugs, you’re at higher risk. And you need a plan.
What’s Being Done-And What You Can Do Now
The National Institute on Aging is funding $4.2 million in new research to study how medications affect heat tolerance in older adults. Penn State’s Dr. W. Larry Kenney is leading a $2.8 million NIH study expected to release results in early 2025. The CDC’s Heat and Health Tracking System now includes medication data in 25 U.S. states.
But you don’t have to wait for a government study to save your life. Start today:
- Make a list of every medication you take, including over-the-counter ones.
- Look up each one’s anticholinergic burden score online (ACB scale: 0 = no effect, 1 = mild, 2 = moderate, 3 = strong).
- Call your pharmacist or doctor and ask: “Which of these could make me vulnerable to heat?”
- Designate a family member, neighbor, or friend to check on you daily during hot weather.
- Keep a thermometer in your home. If it hits 77°F (25°C), start taking extra precautions.
Heat doesn’t care if you’re taking medicine for your heart, your bladder, or your mood. It only cares if your body can cool down. And if your meds are stopping you from sweating or holding water, you’re one heatwave away from disaster.
Don’t risk it. Talk. Adjust. Prepare. Your life depends on it.
Can I stop taking my diuretic if it’s too hot?
No. Stopping your diuretic without medical advice can cause dangerous fluid buildup, high blood pressure, or heart failure flare-ups. Instead, talk to your doctor about adjusting your dose or timing during hot weather. Never make changes on your own.
Do all anticholinergic drugs stop sweating the same amount?
No. Drugs are ranked on the Anticholinergic Burden (ACB) scale: 0 (no effect), 1 (mild), 2 (moderate), or 3 (strong). Oxybutynin, tolterodine, amitriptyline, and diphenhydramine (Benadryl) are ACB=3 and significantly reduce sweating. Others like loratadine (Claritin) are ACB=0 and pose little to no risk. Check your specific medication’s ACB score.
Is it safe to use a fan if I’m on these medications?
Yes. Fans help evaporate sweat and cool your skin-even if you’re sweating less. But if the temperature is above 95°F (35°C), a fan alone won’t be enough. Use air conditioning if possible. If you don’t have it, go to a cooling center, library, or mall.
What should I do if I feel dizzy or confused in the heat?
Stop what you’re doing, move to a cool place, drink water slowly, and call 999 or go to the nearest emergency department. Dizziness and confusion are signs of heat exhaustion or heat stroke-both medical emergencies. Don’t wait to see if it gets better.
Are there alternatives to anticholinergics for overactive bladder?
Yes. Options include beta-3 agonists like mirabegron (Myrbetriq), pelvic floor therapy, bladder training, or Botox injections. These don’t block sweating and carry less heat risk. Talk to your urologist or GP about switching if you’re at high risk for heat illness.
Can I still go outside if I’m on these medications?
Yes-but be smart. Avoid being outside between 10 a.m. and 4 p.m. When you go out, wear a wide-brimmed hat, carry water, and stay in the shade. Limit time outdoors to under 30 minutes on hot days. Always have someone know where you are.

Comments (14)
Zed theMartian
December 1, 2025 AT 20:09Oh wow, another ‘heat is dangerous’ article. Next you’ll tell me breathing oxygen is risky if you’re on beta-blockers. At this point, we’re just medicalizing common sense. People have lived through summers for millennia without CDC pamphlets. If you’re on diuretics and you’re dumb enough to run a marathon in 90°F, maybe don’t blame the meds-blame your poor life choices.
Ella van Rij
December 1, 2025 AT 20:44sooo… like… uhhh… i read this whole thing and now i’m scared to drink water?? 🤔 also, who decided ‘dry skin = emergency’? my skin is always dry. even in winter. also, is this article sponsored by the AC brand? just asking for a friend who’s about to sell her house to buy a portable AC unit.
ATUL BHARDWAJ
December 3, 2025 AT 04:36Heat kills. Medications make it worse. Simple. No need for charts. No need for scores. Just drink water. Stay cool. Talk to doctor. Done.
Rebecca M.
December 3, 2025 AT 19:31Oh my god. I just realized my grandma takes oxybutynin AND hydrochlorothiazide. She also walks her poodle at 2 p.m. in Florida. I’m calling her right now. And then I’m calling 911. And then I’m moving her to Alaska. With me. And a fan. And a lifetime supply of Gatorade.
मनोज कुमार
December 5, 2025 AT 07:50ACB score is meaningless without pharmacokinetic modeling. The real issue is CYP450 interactions and thermoregulatory thresholds under polypharmacy. Also, most studies are on young males. Your data is garbage. And your advice is performative.
Jack Dao
December 6, 2025 AT 20:50People like you who write these posts think you’re saving lives. You’re not. You’re just making anxious people feel worse. I’ve been on amitriptyline for 15 years. I live in Arizona. I sweat less. I’m fine. Stop scaring people into buying $500 air conditioners. Some of us have lived through worse.
Also, why is everyone suddenly terrified of heat? It’s not 2021 anymore. It’s 2025. We’re not all dying in our living rooms. Get a fan. Wear a hat. Drink water. You’re not a lab rat.
And if you’re taking Benadryl for sleep and then panic about sweating? Yeah. That’s on you. Not the CDC.
dave nevogt
December 8, 2025 AT 19:33There’s a quiet tragedy here that no one talks about: the erosion of bodily autonomy under medicalized fear. We’re told to drink water even when not thirsty, to fear the sun, to distrust our own sensations because a drug has altered our perception. But what does it mean to live in a body that no longer signals truthfully? Is safety just the absence of danger-or the surrender of self-trust? I wonder if the real cost of these medications isn’t just the physical risk, but the psychological weight of never feeling safe in your own skin. Even when the air is still, even when the shade is cool-you’re still waiting for the next symptom. The next collapse. The next call to 999. And that silence? That’s the loudest thing of all.
Arun kumar
December 10, 2025 AT 07:33good article but i think we need more focus on cultural context. in india we dont have ac in 70% homes but people still survive. maybe the issue is not just meds but lack of public cooling spaces. also, why no mention of traditional cooling drinks like jal jeera or buttermilk? they help more than you think. and yes, i take amitriptyline and i drink water every hour. its not hard.
Jay Everett
December 10, 2025 AT 14:54Y’all need to stop treating this like a horror movie. This isn’t ‘The Heat Is Coming for You.’ This is ‘Your Body Has a Manual, and You Forgot to Read It.’
Here’s the deal: If you’re on meds that mess with sweat or fluid balance, you’re not ‘at risk’-you’re just playing a harder version of the game. You need a new strategy. Not panic. Not avoidance. Strategy.
Step 1: Know your meds. Use the ACB scale. Google it. It’s free.
Step 2: Set phone alarms for water. Every hour. Even if you’re watching Netflix.
Step 3: Wear white. Cotton. Hat. Sunglasses. No excuses.
Step 4: Have a ‘heat buddy.’ Someone who texts you at 2 p.m. every day. If you don’t reply? They call 911. No drama.
And if you’re still on diphenhydramine for sleep? Please. Stop. It’s 2025. There are better options. Your brain deserves more than a ghost in a jar.
Joel Deang
December 11, 2025 AT 02:44so i read this and now im scared to go outside… but also i think the acb scale is kinda sus? like… i looked up my meds and it says ‘moderate’ but my aunt took the same one and she’s fine? maybe its just… you know… being old? also, i think the author forgot about people who dont have ac and dont make enough to buy it. like… what do they do? go to the library? yeah right. my town has one but its closed on tuesdays. and its 90 degrees. so… yeah.
Roger Leiton
December 12, 2025 AT 05:39Can we talk about how the CDC’s tracking system only covers 25 states? What about the rest? What about rural areas? What about people without smartphones to check ACB scores? This feels like a rich-person safety guide. I live in a town where the nearest cooling center is 40 miles away. My car doesn’t have AC. My meds are on a $5 generic plan. So… what’s my plan? 😔
Laura Baur
December 12, 2025 AT 19:43It’s not just about the meds. It’s about the systemic abandonment of elderly, chronically ill, and low-income populations. The fact that we need to ‘designate a buddy’ to prevent death from heat exposure reveals a societal failure far deeper than pharmacology. We have allowed the commodification of health to the point where survival depends on personal vigilance, not public infrastructure. This isn’t a medical advisory. It’s a eulogy for a society that no longer believes in collective care. And yet, we’re told to ‘just drink water.’ As if hydration is a moral choice, not a right. As if your grandmother’s death from heatstroke is a personal failure, not a political one. We have the data. We have the resources. What we lack is the will to act. And that’s the real anticholinergic: apathy.
Steve World Shopping
December 14, 2025 AT 00:42Let me break this down in corporate speak: Heat exposure + polypharmacy = non-optimal thermal homeostasis. Mitigation strategy: reduce ACB burden via pharmacoeconomic substitution. Recommend switching to mirabegron. ROI: 78% reduction in ER visits. Also, your sunscreen is probably expired. Check the batch number.
Jack Dao
December 14, 2025 AT 03:03Rebecca M. said she’s calling her grandma. That’s good. But let’s be real-most people don’t have a Rebecca. Most people have a cousin who texts ‘u ok?’ once a week and then forgets. And the ones who don’t have anyone? They’re the ones who just… disappear. This isn’t about advice. It’s about who gets to be seen. And if your name isn’t on a list, your heatstroke won’t make the news.