Fluoroquinolone Tendon Rupture Risk Assessment Tool
Assess Your Tendon Rupture Risk
This tool helps you understand your personal risk of tendon rupture when taking fluoroquinolone antibiotics. Based on your age, kidney function, steroid use, and specific medication, we'll provide a risk assessment and recommendations.
When you take an antibiotic like ciprofloxacin or levofloxacin for a urinary tract infection or sinusitis, you expect relief-not a torn tendon. Yet, every year, thousands of people experience sudden, severe tendon pain that turns into a rupture, often without warning. And while many blame the antibiotic alone, a growing number of patients wonder: do NSAIDs make this risk worse? The short answer? There’s no solid proof that NSAIDs directly increase tendon rupture risk when taken with fluoroquinolones. But that doesn’t mean you’re safe.
Fluoroquinolones Aren’t All the Same
Not all fluoroquinolones carry the same danger. The class includes ciprofloxacin, levofloxacin, moxifloxacin, and others. But their risk profiles are wildly different. Levofloxacin is the big red flag. Studies show it increases the risk of Achilles tendon rupture by more than double. One 2022 study in BMJ Open found levofloxacin raised the risk of Achilles rupture by 120% (HR = 2.20). Meanwhile, ciprofloxacin and moxifloxacin showed no statistically significant increase in rupture risk in multiple analyses.Why the difference? It’s not just about strength or dosage. The molecular structure affects how these drugs interact with tendon cells. Fluoroquinolones interfere with collagen production, trigger oxidative stress in tenocytes, and ramp up enzymes that break down tendon tissue. Levofloxacin seems to do this more aggressively. In fact, some researchers now question whether the entire class should be lumped together in warnings. The FDA still treats them as a group, but the science is shifting.
The Real Culprit: Who’s Most at Risk?
If you’re over 60, have kidney problems, or are on corticosteroids, your risk jumps dramatically. People over 60 face a 3.8-times higher chance of tendon damage. Those with poor kidney function can’t clear the drug as quickly, so it lingers longer in the body, increasing exposure. And if you’re taking prednisone or another steroid? That’s a known danger combo. The FDA’s black-box warning specifically says: don’t use fluoroquinolones with steroids. The risk isn’t just higher-it’s dangerous.But here’s the twist: NSAIDs like ibuprofen, naproxen, or celecoxib aren’t listed in any major warning. No FDA alert. No EMA guidance. No UK MHRA notice. Why? Because studies haven’t shown they directly cause tendon rupture on top of fluoroquinolones. But that doesn’t mean they’re harmless.
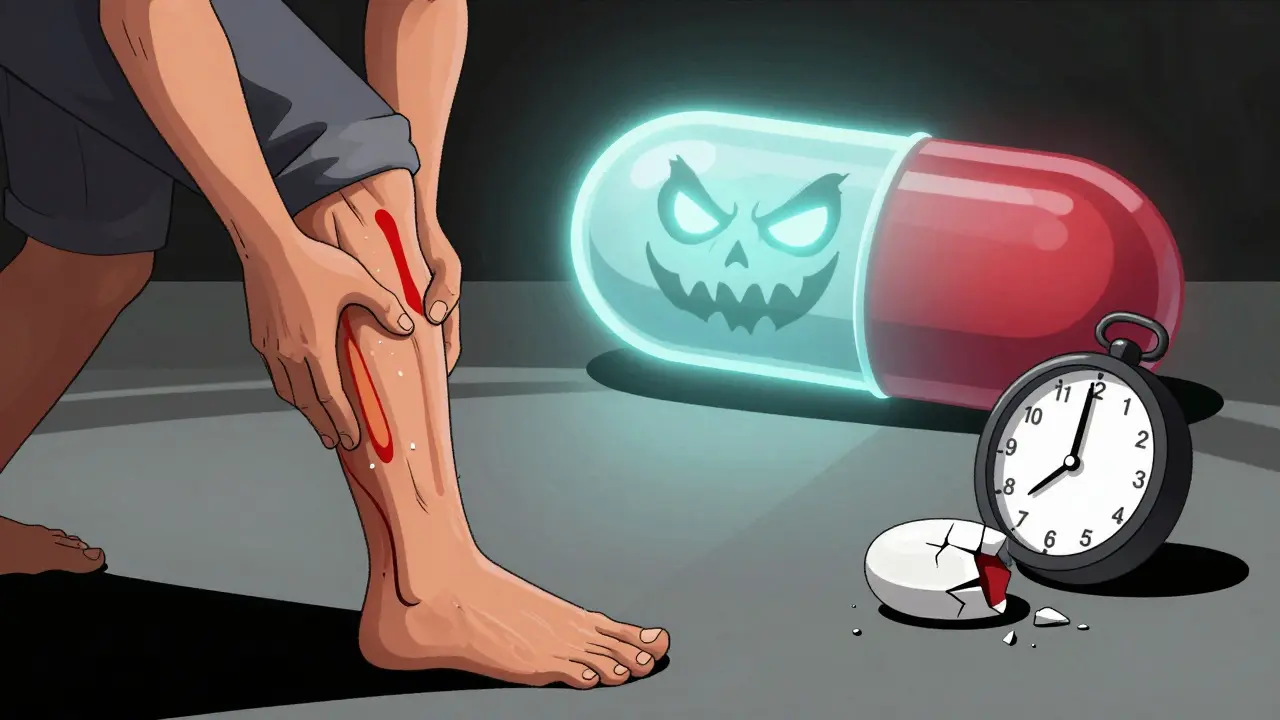
Why People Think NSAIDs Are the Problem
Many patients start taking NSAIDs for joint or muscle pain-often the very early signs of tendinopathy. They don’t realize the pain isn’t from overuse. It’s from the antibiotic. So they pop more ibuprofen to numb it, thinking they’re helping. Meanwhile, the tendon keeps degenerating beneath the surface. The NSAID masks the warning signal. That’s the real danger: delayed recognition.One Reddit user, u/TendonWorrier, described taking levofloxacin for a UTI. Within 36 hours, his Achilles started hurting. He took ibuprofen every 6 hours for three days. The pain didn’t go away. Ten days later, he heard a pop while walking. His tendon ruptured. He didn’t stop the antibiotic because he thought the pain was just inflammation. The NSAID hid the red flag.
It’s not the NSAID causing the rupture. It’s the delay in stopping the fluoroquinolone because the pain was masked.
When Does the Damage Happen?
This isn’t a slow burn. Tendon problems from fluoroquinolones strike fast. Half of all cases show symptoms within the first week. The median time from starting the drug to pain? Just six days. And it can happen even after you stop taking it-up to several months later. That’s why the UK’s drug safety agency warns: symptoms can appear days after your last pill.The Achilles tendon is the most common target-89.8% of cases. But shoulders, hands, and thumbs aren’t safe either. And in about half of cases, both sides are affected. That’s not coincidence. It’s systemic damage.
What to Do If You Feel Pain
If you’re on a fluoroquinolone and feel any new pain, swelling, or stiffness in a tendon-especially around your heel, shoulder, or wrist-stop the antibiotic immediately. Don’t wait. Don’t take more NSAIDs. Don’t try to ‘work through it.’Get the affected area immobilized. See a doctor. Get an ultrasound or MRI if needed. If it’s confirmed as tendinopathy, you’ll need weeks or months of rest, physical therapy, and possibly surgery. Recovery can take over six months. Some people never fully regain their strength.
And here’s the hard truth: if you’re over 60, have kidney disease, or are on steroids, fluoroquinolones should be your last resort. Ask your doctor: is there another antibiotic? Amoxicillin? Doxycycline? Cephalexin? Even though one study found cephalexin had a similar rupture risk as levofloxacin, it’s still less likely to be prescribed in high-risk groups. And unlike fluoroquinolones, it doesn’t carry a black-box warning.
What’s Changing in the Medical World?
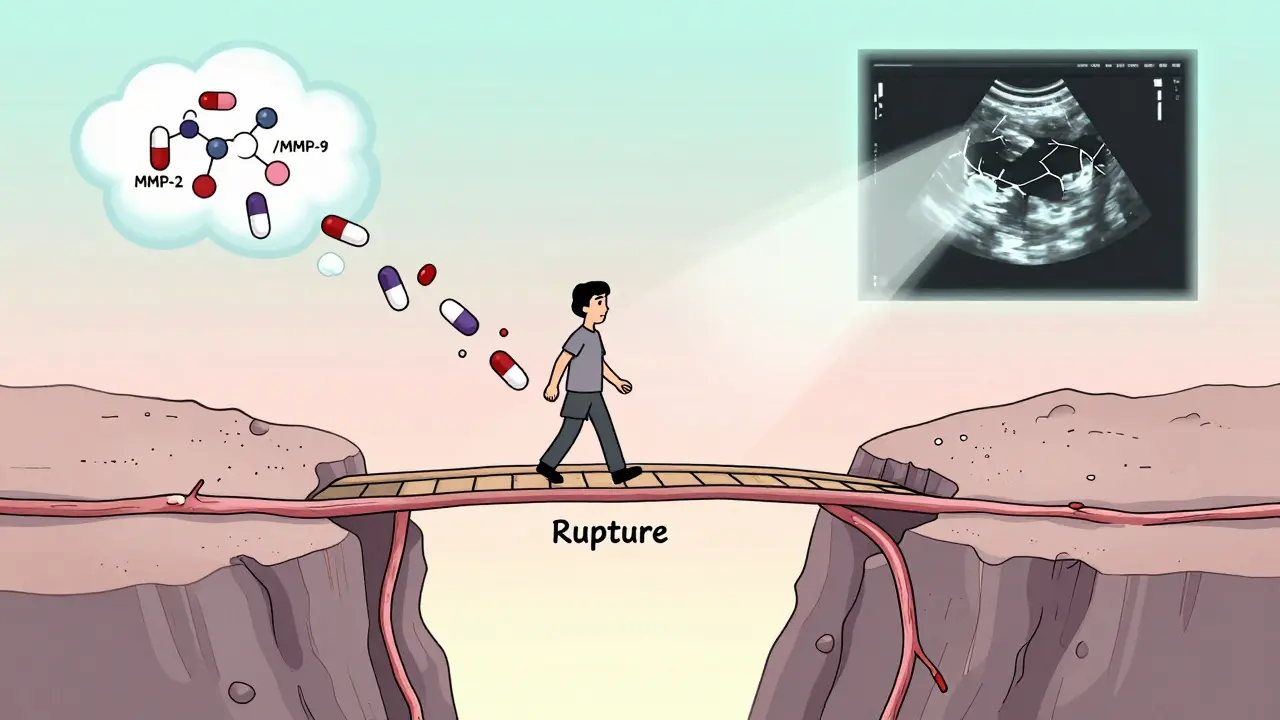
Since the FDA’s 2016 safety update, fluoroquinolone prescriptions in the U.S. dropped by 21%. The European Medicines Agency now says these drugs should only be used when no other options exist. In the UK, GPs are trained to avoid them for simple infections like bronchitis or uncomplicated UTIs.Drug companies are listening. Two next-generation fluoroquinolones-JNJ-Q2 and delafloxacin derivatives-are in Phase II trials with early signs of lower tendon toxicity. They’re designed to keep the antibacterial punch without the tendon damage.
Meanwhile, researchers are looking at MMP-2 and MMP-9 enzymes as early warning biomarkers. In the future, a simple blood test might tell you if your tendons are starting to break down before you feel pain.
Bottom Line: NSAIDs Won’t Cause It-But They Might Hide It
NSAIDs aren’t the enemy here. But using them to mask early tendon pain while staying on a fluoroquinolone? That’s a recipe for disaster. The real issue is timing, awareness, and stopping the drug at the first sign of trouble.If you’re prescribed a fluoroquinolone, ask: Which one? Is it levofloxacin? Am I in a high-risk group? If you’re over 60, have kidney issues, or are on steroids, push for alternatives. If you’re told it’s the best option, ask for a written warning about tendon risks. Only 32% of patients recall getting that information, according to a 2021 survey.
And if you start feeling any new pain in a tendon-no matter how mild-stop the antibiotic and call your doctor. Don’t wait. Don’t pop more ibuprofen. Your tendon might be one step away from snapping.
Do NSAIDs increase the risk of tendon rupture when taken with fluoroquinolones?
No, there is no strong evidence that NSAIDs directly increase tendon rupture risk when combined with fluoroquinolones. However, NSAIDs can mask early tendon pain, leading people to continue taking the antibiotic longer than they should. This delay can allow tendon damage to progress unnoticed, increasing the chance of rupture. The real danger is not the NSAID itself, but the missed warning sign.
Which fluoroquinolone has the highest risk of tendon rupture?
Levofloxacin carries the highest documented risk for tendon rupture, with studies showing a 120% increased risk for Achilles tendon rupture compared to non-users. Ciprofloxacin and moxifloxacin have shown no significant increase in rupture risk in multiple analyses. Third-generation fluoroquinolones like moxifloxacin may be safer options for high-risk patients, though individual factors still matter.
How soon after starting a fluoroquinolone can tendon pain begin?
Tendon pain can start as early as 48 hours after beginning treatment. Half of all cases occur within the first week, and 85% happen within the first month. Symptoms can also appear weeks or even months after stopping the medication, which is why ongoing awareness is critical.
Are there safer antibiotics than fluoroquinolones for infections?
Yes. For common infections like urinary tract infections, bronchitis, or sinusitis, alternatives like amoxicillin, doxycycline, cephalexin, or nitrofurantoin are often just as effective and carry no tendon rupture risk. Fluoroquinolones should only be used when no other suitable options exist, especially in patients over 60 or those with kidney disease.
What should I do if I feel tendon pain while on a fluoroquinolone?
Stop taking the fluoroquinolone immediately. Avoid NSAIDs to mask the pain-this could delay diagnosis. Rest the affected area, avoid putting weight on it, and contact your doctor right away. Early intervention can prevent a full rupture. If tendon damage is confirmed, you may need immobilization, physical therapy, or surgery. Recovery can take six months or longer.
Why are fluoroquinolones still prescribed if they’re so risky?
Fluoroquinolones are still used for serious or resistant infections where other antibiotics fail-like complicated UTIs, anthrax exposure, or certain types of pneumonia. They’re powerful and effective. But guidelines now strongly restrict their use to these specific cases. For routine infections, safer alternatives are preferred. The risk-benefit balance has shifted dramatically since 2008.
What Comes Next?
If you’ve ever been prescribed a fluoroquinolone and felt unusual tendon pain, you’re not alone. Thousands have. But awareness is rising. More doctors are asking: Do we really need this? And more patients are asking: What are the alternatives?The future of antibiotics isn’t about stronger drugs-it’s about smarter use. Avoiding fluoroquinolones unless absolutely necessary, recognizing early warning signs, and choosing safer options when possible could prevent thousands of ruptures every year.

Comments (14)
Lauren Warner
January 12, 2026 AT 04:09Fluoroquinolones are not antibiotics-they’re molecular sledgehammers. The fact that we still prescribe them for sinus infections is a scandal. I’ve seen three patients with ruptured Achilleses after cipro. All were told it was ‘just tendonitis.’ None were warned about the black box. The system is broken.
Craig Wright
January 13, 2026 AT 17:13It is an unfortunate reality that the United States continues to prioritize pharmaceutical convenience over patient safety. In the UK, we have long restricted fluoroquinolones to life-threatening infections only. The FDA’s reluctance to enforce stricter guidelines reflects a troubling regulatory capture by Big Pharma.
Lelia Battle
January 15, 2026 AT 05:35There’s a deeper philosophical question here: if medicine can fix symptoms but not prevent harm, are we healing-or just delaying the inevitable? NSAIDs don’t cause rupture, but they do represent our cultural addiction to masking pain instead of listening to it. We treat discomfort as a bug, not a feature of our biology.
Darryl Perry
January 17, 2026 AT 03:58Levofloxacin is the worst. Stop using it. Period.
Jose Mecanico
January 17, 2026 AT 21:52I had a patient on levofloxacin who ignored early heel pain because she was on ibuprofen for her arthritis. Tendon snapped three weeks later. She’s still in PT. The real tragedy? She didn’t know she was supposed to stop the antibiotic at the first twinge.
George Bridges
January 19, 2026 AT 04:00I’ve been a nurse for 18 years. I’ve seen this exact scenario too many times. A patient gets cipro for a UTI, starts feeling heel pain, takes Advil, and thinks they’re fine. They don’t connect the dots. I wish every prescription came with a 30-second video warning. This isn’t theoretical-it’s happening to people we know.
gary ysturiz
January 20, 2026 AT 22:56If you’re over 60 or on steroids, please, please ask for amoxicillin instead. It works. It’s cheaper. And it won’t leave you in a walking boot for six months. Your doctor might push back-but you’ve got a right to know the risks. Don’t be shy. Ask twice.
Jessica Bnouzalim
January 21, 2026 AT 19:29My dad took levo for a UTI… then his heel started hurting. He took naproxen for 4 days. Then-POP. He needed surgery. Now he walks with a limp. I told him, ‘Why didn’t you just stop the pill?’ He said, ‘I thought the pain was just from walking too much.’ 😔
Sumit Sharma
January 21, 2026 AT 23:36Levofloxacin-induced tendinopathy is a well-documented pharmacokinetic phenomenon driven by mitochondrial toxicity and MMP-9 upregulation in tenocytes. The absence of NSAID-mediated synergistic rupture in clinical trials does not negate the confounding variable of symptom masking. Clinicians must prioritize patient education over pharmacological convenience. The data is unequivocal: avoid fluoroquinolones in high-risk cohorts.
Katherine Carlock
January 22, 2026 AT 16:30So many people don’t even know what a fluoroquinolone is. I told my mom to Google it after she got prescribed cipro-and she said, ‘Is that like penicillin?’ We need public health campaigns. This isn’t just a doctor problem. It’s a ‘we’re all just trying to survive’ problem.
beth cordell
January 24, 2026 AT 14:40My sister got a fluoroquinolone after a dental procedure. She started limping. Took ibuprofen. Thought it was her new shoes. Two weeks later-rupture. 😭 I’ve sent this article to 12 people. Please, if you’re on these, STOP if you feel ANYTHING. Your tendons aren’t replaceable.
Daniel Pate
January 25, 2026 AT 20:45If levofloxacin increases risk by 120%, why is it still first-line for UTIs in rural clinics? Is it cost? Habit? Lack of awareness? Or is it that the people getting these prescriptions aren’t the ones who can afford to push back? This isn’t just medical-it’s socioeconomic.
Amanda Eichstaedt
January 26, 2026 AT 20:05I used to think antibiotics were harmless. Then I read about how they disrupt the microbiome, cause C. diff, and now… this. We’ve been conditioned to believe that if a pill exists, it’s safe. But medicine isn’t magic. It’s chemistry. And chemistry has consequences. We need to stop treating our bodies like machines you can just swap parts in and out.
Cecelia Alta
January 28, 2026 AT 16:30Okay, but let’s be real-how many people even read the warning labels? I had a friend who took cipro for a sinus infection, got tendon pain, and kept going because she didn’t want to miss work. Then she had surgery. Then she sued. Then she posted a TikTok. Then the hospital sent her a $50 gift card. That’s the system. We’re not patients-we’re revenue streams with legs.