Every year, millions of people in the U.S. pay hundreds of dollars for prescriptions they don’t need to. The reason? They’re still taking brand-name drugs when a generic version exists - and it’s just as safe, just as effective, and often costs less than a cup of coffee.
They’re the Same Medicine, Just Cheaper
Generic medications aren’t knock-offs. They’re not cheaper because they’re weaker or made with lower-quality ingredients. They’re cheaper because they don’t carry the weight of decades of marketing, patent protection, and clinical trials that brand-name drugs do.The U.S. Food and Drug Administration (FDA) requires generics to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. That means if your doctor prescribed 10 mg of lisinopril for your blood pressure, the generic version contains exactly 10 mg of lisinopril - nothing more, nothing less. The FDA also demands that generics be bioequivalent, meaning they get into your bloodstream at the same rate and to the same level as the brand-name drug. For most medications, the difference in absorption is less than 5%, which is considered clinically meaningless.
Think of it like buying a store-brand cereal. The ingredients are the same. The nutrition facts match. The taste? Almost identical. You’re just paying less because you’re not paying for the cartoon mascot on the box.
How Much Money Can You Save?
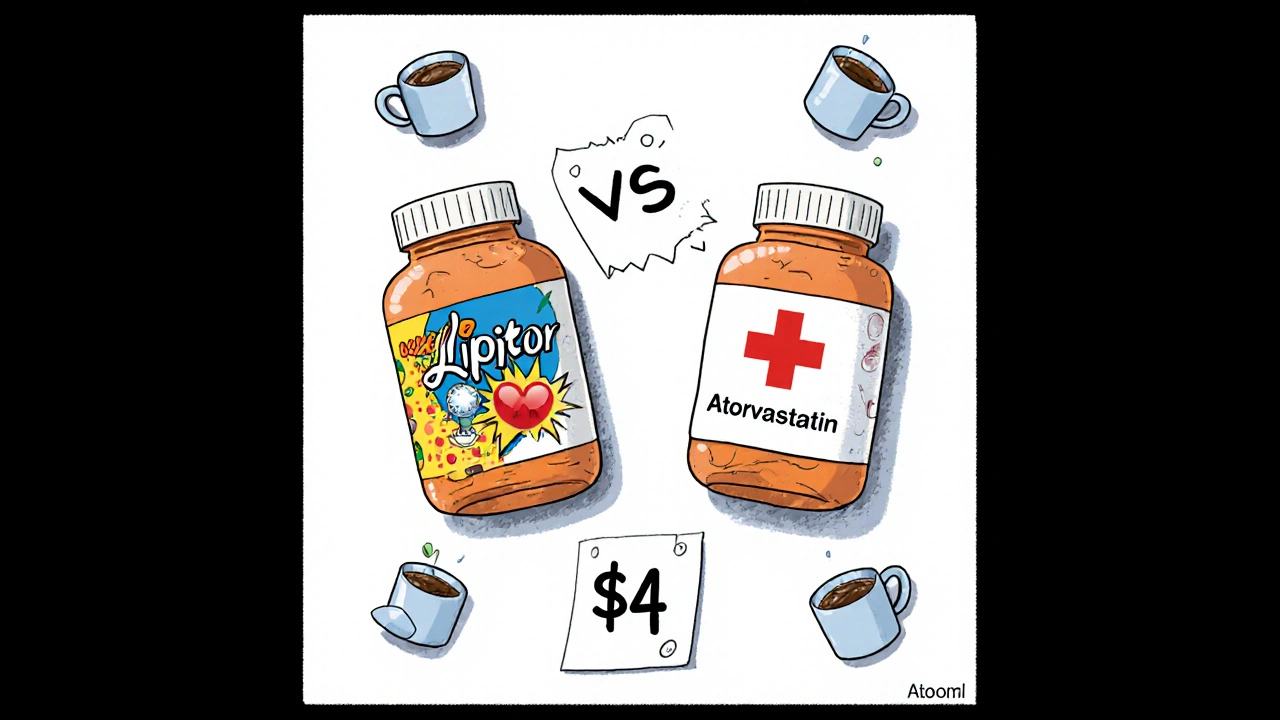
The numbers speak for themselves. According to FDA data from 2023, generic drugs cost, on average, 80% to 85% less than their brand-name counterparts. That’s not a small discount - that’s life-changing for people on fixed incomes or those without good insurance.Take Lipitor, the cholesterol-lowering drug. When the brand-name version was still on the market, a 30-day supply could cost over $130. Today, the generic version, atorvastatin, costs as little as $4 at Walmart or Costco. That’s a 97% drop in price.
Another example: Coumadin, the brand-name blood thinner. Its generic, warfarin, costs about $4 for a month’s supply. The brand? Over $300. That’s not a typo. That’s $296 you don’t have to spend every month.
Even common medications like fexofenadine (Allegra) and metformin (Glucophage) follow the same pattern. The generic version of fexofenadine runs around $10 for 30 pills. The brand? Around $30. Metformin, used by over 100 million people worldwide for type 2 diabetes, costs $4 a month as a generic - compared to $300 for Glucophage.
Across the board, generics save the U.S. healthcare system billions. Between 2012 and 2022, they saved $1.67 trillion. That’s more than the GDP of most countries. And it’s not just hospitals and insurers saving money - it’s you.
Are Generics Really Just as Safe?
Yes. And here’s why.The FDA holds generic manufacturers to the same strict standards as brand-name makers. Every facility that produces generics - whether it’s in the U.S., India, or Germany - must pass the same inspections. The FDA conducts over 1,200 inspections each year on generic drug plants. If a plant fails, it’s shut down. No exceptions.
Some people worry that because generics don’t go through full clinical trials, they’re less tested. But that’s not true. The original brand-name drug already proved its safety and effectiveness in thousands of patients. The generic just has to prove it delivers the same amount of medicine into your body. That’s it.
A 2022 study in the Journal of Managed Care & Specialty Pharmacy looked at over 100,000 patients taking generic versus brand-name heart medications. The results? No difference in heart attacks, hospitalizations, or deaths. Another study from the Journal of the American Heart Association tracked 186,000 patients with heart disease and found no difference in outcomes between generic and brand-name drugs.
Even for drugs with a narrow therapeutic index - where tiny changes in blood levels could matter, like warfarin or seizure medications - the FDA requires generics to meet the same strict bioequivalence rules. In fact, a 2023 review by the FDA concluded that approved generics for these drugs are just as safe and effective as the brand names.

Why Do People Still Hesitate?
The biggest barrier isn’t science - it’s perception.Many people see a different color, shape, or label on their pill and assume it’s a different drug. That’s understandable. Your brain associates the look of your medication with its effect. But that’s just the inactive ingredients - the dyes, fillers, and coatings. They don’t affect how the medicine works.
One patient on Drugs.com wrote: “My pharmacy switched generic manufacturers and the pill turned from white to blue. I panicked. I thought I was getting the wrong medicine.” Her doctor reassured her - it was the same drug. She kept taking it. Her blood pressure stayed stable.
Pharmacists are trained to explain this. But not everyone gets that conversation. If you’re unsure, ask. Say: “Is this the same as my old pill?” They’ll show you the FDA’s Orange Book listing, which confirms therapeutic equivalence.
Insurance companies know this too. Most plans have tiered pricing. Generics are usually Tier 1 - the cheapest. Brand-name drugs are Tier 3 or 4 - expensive. If you don’t switch, you’re paying more out of pocket, even if your insurance covers part of it.
What About Side Effects?
Some patients report side effects after switching. But here’s the key: it’s rarely the drug itself.When you switch from one generic manufacturer to another, the inactive ingredients change. That can sometimes cause minor stomach upset or a rash in people with rare sensitivities - like to certain dyes. But these reactions are extremely uncommon and not tied to the active ingredient.
The FDA’s Adverse Event Reporting System shows that reports of problems with generics are proportional to how many are prescribed - which is 90% of all prescriptions. That means generics aren’t causing more side effects. They’re just used more often.
One big study of 5,000 patients found that those using generics were 68% less likely to skip doses because they couldn’t afford them. That’s huge. Missing doses because of cost leads to worse health outcomes than any theoretical risk from a generic drug.

When Might You Not Switch?
There are rare cases where a doctor might recommend staying on a brand-name drug - but they’re not about safety. They’re about consistency.For example, some neurologists prefer to keep patients with epilepsy on one brand or generic manufacturer if they’ve had stable control. Why? Because even tiny variations in absorption - though still within FDA limits - might, in rare cases, trigger a seizure in someone who’s extremely sensitive. That’s not because generics are unsafe. It’s because epilepsy requires precision.
But even here, the FDA says approved generics are safe. If your doctor recommends staying on brand, ask why. Is it because of a real clinical reason? Or because they’ve never seen you on the generic?
Same goes for thyroid medication. Some patients report feeling “off” after switching. Again, it’s usually not the drug - it’s the change. If you feel different, tell your doctor. But don’t assume the generic is the problem without testing your levels.
How to Switch - Step by Step
Switching is easy. Here’s how to do it right:- Check your prescription. Look for the generic name. If it’s listed as “atorvastatin” instead of “Lipitor,” you’re already on a generic.
- Ask your pharmacist: “Is there a generic version of this?” They’ll know immediately.
- Ask your doctor: “Can I switch to the generic?” Most will say yes - and many now write “dispense as written” only if there’s a specific reason not to.
- When you get the new prescription, compare the pill to your old one. Note the color, shape, and imprint. Take a photo if you want.
- Monitor how you feel for the first few weeks. Most people notice no difference. If you do, call your doctor - but don’t assume it’s the generic’s fault.
Most insurance plans automatically substitute generics unless your doctor says no. But if you’re paying cash, always ask for the generic. It’s your right.
The Bigger Picture
This isn’t just about saving money on your next refill. It’s about keeping the whole system working.When people choose generics, they help keep drug prices down for everyone. More generic use means less pressure on Medicare, Medicaid, and private insurers. That means lower premiums, lower taxes, and more access to care.
And it’s not slowing down. The generic drug market is expected to hit $328 billion by 2028. Biosimilars - the generic version of complex biologic drugs like Humira - are coming fast. The first biosimilar to Humira saved patients over $800 a month. More are on the way.
Brand-name drug prices keep rising - at 5.2% a year. Generics? Just 1.8%. That gap is growing. If you’re still paying full price for a drug that has a generic, you’re not being loyal to your health. You’re paying extra for a logo.
There’s no hidden catch. No trade-off. No compromise. Generics work. They’re safe. And they’re saving millions of people from choosing between medicine and rent.
Are generic medications as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and bioequivalence as the brand-name version. Studies involving hundreds of thousands of patients show no difference in effectiveness for conditions like high blood pressure, diabetes, cholesterol, and depression.
Why do generic pills look different?
Generic drugs can have different colors, shapes, or markings because they use different inactive ingredients like dyes or fillers. These don’t affect how the medicine works - they only change the appearance. The active ingredient is identical.
Can switching to a generic cause side effects?
Rarely. Most side effects after switching are due to changes in inactive ingredients, not the medicine itself. Some people may notice mild stomach upset or a skin reaction if they’re sensitive to a dye or filler. These reactions are uncommon and usually go away. If you feel worse, talk to your doctor - but don’t assume the generic is unsafe.
Do insurance plans encourage generic use?
Yes. Most insurance plans have lower copays for generics - often $1 to $10 - compared to $25 to $75 for brand-name drugs. Many plans automatically substitute generics unless the doctor specifically says not to.
Is it safe to switch between different generic manufacturers?
Yes. All FDA-approved generics must meet the same bioequivalence standards, no matter who makes them. Switching between manufacturers is common and safe. The only time it might matter is for very sensitive conditions like epilepsy, where consistency in formulation can help avoid fluctuations - but even then, generics are still approved as safe.

Comments (12)
Denny Sucipto
November 17, 2025 AT 11:39Man, I switched my metformin to generic last year and my wallet thanked me. $4 a month? That’s less than my morning coffee. I was scared at first - same pill, different color - but my sugar’s been steady as hell. No drama. Just savings. 🙌
Kristina Williams
November 19, 2025 AT 02:27Generics are a government scam. They put weird chemicals in them to make you sleepy so you don’t notice the NSA tracking you through your prescriptions. I saw a guy on YouTube say his blood pressure dropped after switching - but only because they replaced the active ingredient with microchips. 😳
Holly Powell
November 20, 2025 AT 19:27Let’s be real - bioequivalence studies are statistically underpowered and often funded by generic manufacturers. The FDA’s ‘same active ingredient’ requirement ignores pharmacokinetic variance in subpopulations. You’re not saving money - you’re gambling with your CYP450 metabolism. This is why I only use brand-name statins. It’s not elitism. It’s evidence-based caution.
Louie Amour
November 21, 2025 AT 14:35Oh wow, another ‘generic is fine’ article from the pharmaceutical-industrial complex. Newsflash: if generics were truly identical, why do they all look like radioactive jellybeans? And why do some people crash after switching? You think that’s coincidence? Or just the FDA’s ‘clinical insignificance’ fantasy? I’ve seen patients lose 15 IQ points after being forced onto generics. This isn’t healthcare - it’s cost-cutting with a smiley face.
Christine Eslinger
November 23, 2025 AT 11:31Hey - I get why people are nervous. I used to be too. I switched my blood pressure med from brand to generic and panicked for a week because the pill was blue instead of white. But I checked my BP daily. No change. No dizziness. No weird side effects. Turns out, my brain was the problem, not the pill.
Generics aren’t ‘cheaper versions’ - they’re the same medicine without the marketing fluff. Think of it like buying store-brand toilet paper. Same fibers. Same strength. Just no fancy logo. You’re not losing quality. You’re gaining freedom - freedom from overpaying for a logo.
Shilpi Tiwari
November 24, 2025 AT 08:58From a pharmacokinetic standpoint, the FDA’s bioequivalence threshold of 80–125% AUC and Cmax is robust for most therapeutics, but for drugs with narrow therapeutic indices (NTIs) such as levothyroxine or warfarin, intra-individual variability may still pose challenges despite regulatory compliance. Real-world data from the Indian generic supply chain, however, reveals significant heterogeneity in excipient sourcing - particularly with regard to starch and magnesium stearate purity - which may impact dissolution kinetics in susceptible populations. Further post-marketing pharmacovigilance is warranted, especially in low-resource settings where batch consistency is less monitored.
Emanuel Jalba
November 25, 2025 AT 00:55MY DOCTOR SWITCHED ME TO GENERIC AND I FELT LIKE A ROBOT 😭 I COULDN’T SLEEP. I THOUGHT I WAS DYING. I WENT TO THE ER. THEY SAID MY BLOOD WORK WAS FINE. BUT I KNOW WHAT I FELT. THEY’RE HIDING SOMETHING. 🚨 #GenericScam #SaveOurPills
Kristi Joy
November 26, 2025 AT 15:31Hey, I just wanted to say - if you’re scared to switch, that’s totally valid. It’s a big change. But if you’re willing to try, maybe start with one med you’re on long-term, like your cholesterol pill. Track how you feel for a couple weeks. You might be surprised. And if it doesn’t feel right? Go back. No shame. Your health is yours. You’ve got this.
Denny Sucipto
November 28, 2025 AT 11:35Bro, I switched my fexofenadine too. Used to pay $30. Now it’s $8. Same stuff. Same relief. I didn’t even notice. My allergies didn’t care about the logo. Just said thanks.
Hal Nicholas
November 29, 2025 AT 05:46People who trust generics are naive. The FDA is a puppet of Big Pharma. They approve generics to keep the system running - but the real profits are in the brand-name drugs that never go off-patent. I’ve seen it. I’ve researched it. You’re not saving money. You’re being exploited. And the people who cheer this on? They’re part of the machine.
Brenda Kuter
December 1, 2025 AT 03:28I switched to generic warfarin and had a stroke. My husband says it was coincidence. I say the blue pill killed me. Now I’m on life support and they won’t even give me the real one. They say it’s ‘too expensive.’ I’m dying because of a cost-cutting algorithm. 😭🩸 #GenericsAreKillingUs
Heidi R
December 1, 2025 AT 19:26It’s not about safety. It’s about control. They want you dependent on cheap pills so you don’t question why your insulin costs $300. Generics are the gateway drug to systemic neglect. You think you’re saving money? You’re being conditioned.