Drug Interaction Checker
Disclaimer: This tool provides general information only. It is not medical advice. Always consult your doctor or pharmacist about potential interactions.
Take two pills at once - one for blood pressure, another for cholesterol. Seems harmless, right? But what if that simple combo turns a mild headache into a life-threatening bleed? This isn’t rare. Every day, thousands of people experience worse side effects not because their meds are broken, but because they interact.
Why Some Pills Make Other Pills Dangerous
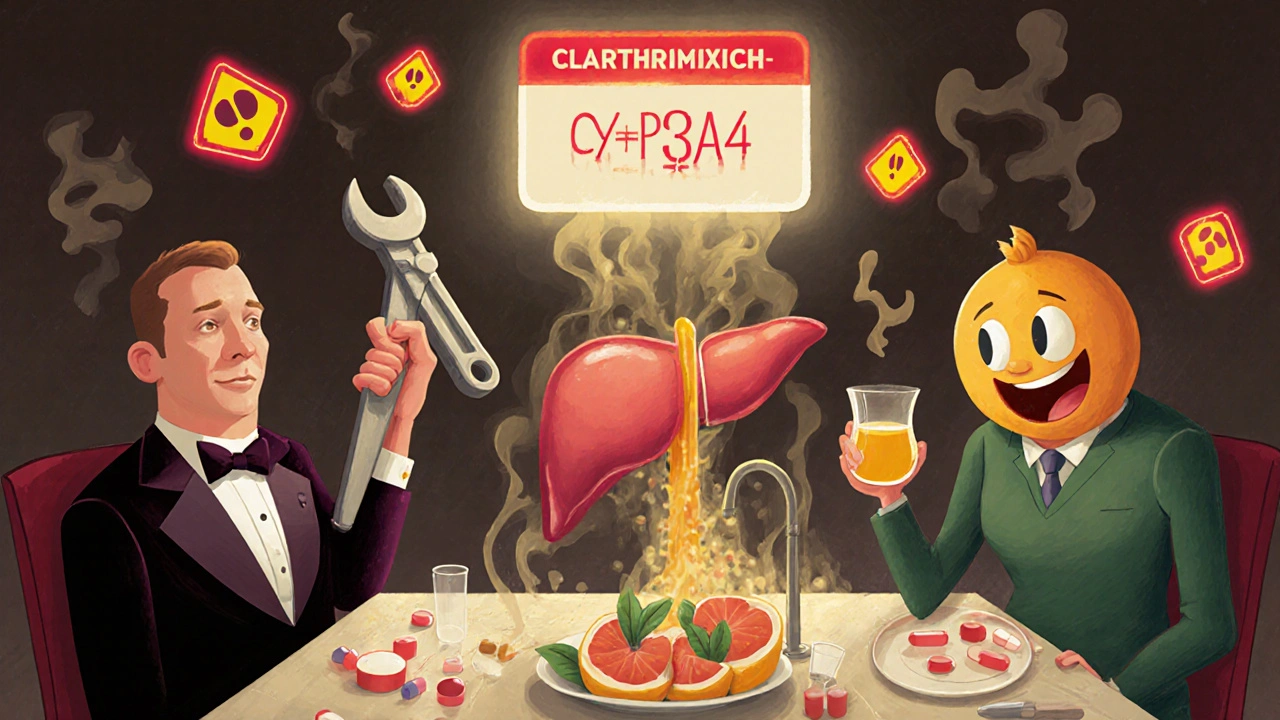
Medications don’t work in isolation. Your body treats them like guests at a dinner party - some get along, others start fights. When two drugs clash, they can turn a manageable side effect into something dangerous. This isn’t guesswork. It’s science.The biggest culprit? The liver. Specifically, a group of enzymes called cytochrome P450. One of them, CYP3A4, handles about half of all prescription drugs. When a second drug blocks or overloads this enzyme, the first drug builds up like a clogged drain. Statins, for example, can spike to 8 times their normal level when taken with clarithromycin. That’s not just a bump in side effects - it’s a 9-fold jump in muscle damage risk, sometimes leading to rhabdomyolysis, a condition that can wreck your kidneys.
It’s not just about the liver. Some drugs bind to calcium in dairy, making antibiotics like tetracycline useless. Others get pushed around by proteins in your blood, changing how much actually reaches your target. And then there’s the gut - grapefruit juice is infamous for blocking enzymes that break down blood pressure meds like felodipine. One glass can triple its concentration. That’s not a myth. That’s a documented spike in low blood pressure, dizziness, and even heart rhythm problems.
High-Risk Combinations You Might Not Know About
Some combinations are so dangerous they’ve been pulled from the market. Cisapride, a stomach drug, was removed after it caused 80 deaths when mixed with common antibiotics like erythromycin. Why? It lengthened the heart’s electrical cycle - a condition called QT prolongation - and when combined with CYP3A4 blockers, that risk jumped 15 times. Patients didn’t know they were playing Russian roulette with their hearts.
Warfarin, a blood thinner, is another silent killer when misused. Add aspirin? Bleeding risk spikes 70-100%. Take too much acetaminophen (more than 2 grams a day)? That also boosts bleeding risk by nearly 80%. Even vitamin K supplements - often taken for bone health - can make warfarin useless. One patient I read about had her INR drop from 3.2 to 1.1 in three days after starting a daily green smoothie. She ended up with a stroke.
Antidepressants and painkillers are another trap. Mixing SSRIs like sertraline with tramadol can trigger serotonin syndrome - a dangerous surge in brain chemicals that causes fever, seizures, and muscle rigidity. In 2023, Reddit users reported 19 verified cases of this combo causing hospitalizations. No one warned them. They just followed their prescriptions.
Why Your Doctor Might Miss It
You’d think doctors know all this. But here’s the problem: there are over 1,500 known drug interactions. No human can memorize them all. Electronic health records flood clinicians with alerts - 90% of which are low-risk or irrelevant. A 2019 JAMA study found that 40% of these alerts are noise. Doctors start ignoring them. They call it alert fatigue. And when they tune out, the real dangers slip through.
Worse, patients rarely tell their doctors about supplements. One 2022 study found that 68% of hospitalized patients had at least one dangerous interaction - and nurses caught 40% of them that doctors missed. Why? Because patients didn’t mention they were taking St. John’s wort for anxiety, or fish oil for heart health, or turmeric for joint pain. Those aren’t “medications” in their mind. But they are in yours.

Who’s Most at Risk?
If you’re taking five or more medications, your risk of a bad reaction jumps 78%. With ten or more? It skyrockets to 153%. That’s not a small increase. That’s a crisis. Older adults, chronic disease patients, and those seeing multiple specialists are the most vulnerable. They’re the ones getting prescriptions from cardiologists, neurologists, rheumatologists - each focused on one problem, not the whole picture.
Genetics play a role too. About 5-10% of white people can’t process codeine properly because they lack the CYP2D6 enzyme. For them, codeine doesn’t just fail to work - it turns into a dangerous overdose. Same with clopidogrel: if you’re a poor metabolizer, the drug won’t prevent clots at all. And most doctors never test for it.
What You Can Do - Right Now
You don’t need to be a pharmacist to protect yourself. Here’s what actually works:
- Make a complete list - every pill, patch, vitamin, herb, and supplement. Include dosages and why you take them. Update it every time something changes.
- Bring it to every appointment - even if you think it’s “just a vitamin.” Tell your doctor, your pharmacist, your nurse. Don’t assume they’ll ask.
- Ask two questions: “Could this interact with anything else I’m taking?” and “Is there a safer alternative?”
- Use free tools - the FDA’s Table of Substrates, Inhibitors and Inducers is public. So is the University of Washington’s Drug Interaction Database. Type in your meds. See what pops up.
- Know your grapefruit warning - if your drug label says “avoid grapefruit,” it’s not a suggestion. It’s a warning. Same for alcohol, St. John’s wort, and black licorice.

The Future Is Personal
Science is catching up. AI models now predict dangerous interactions with 89% accuracy - far better than old databases. Hospitals in the U.S. are starting to test patients for genetic risks before prescribing. Some are even testing wearable sensors that track how drugs behave in real time. Imagine a patch that tells your doctor your warfarin level every day - no more monthly blood draws.
But until then, the system still relies on you. Not because it’s broken - but because it’s too complex for anyone to manage alone. Your job isn’t to memorize pharmacology. It’s to be the one person who remembers everything you take. And who asks the hard questions.
Side effects aren’t always the drug’s fault. Sometimes, they’re the result of what you didn’t say - or what no one bothered to check. Don’t wait for a hospital visit to learn that lesson.
Can over-the-counter drugs cause dangerous interactions?
Absolutely. Common OTC drugs like ibuprofen, aspirin, and even antacids can interfere with prescription medications. Ibuprofen can reduce the heart-protective effect of low-dose aspirin. Antacids with aluminum or magnesium can block absorption of antibiotics like ciprofloxacin. Even allergy meds like diphenhydramine can worsen drowsiness when mixed with opioids or benzodiazepines. Just because it’s sold without a prescription doesn’t mean it’s safe with your other meds.
Are herbal supplements safer than prescription drugs?
No. Supplements like St. John’s wort, garlic, ginkgo, and echinacea are powerful and poorly regulated. St. John’s wort can reduce the effectiveness of birth control, antidepressants, and even HIV meds by speeding up liver metabolism. Garlic and ginkgo thin the blood - dangerous if you’re on warfarin or about to have surgery. Many patients assume “natural” means safe, but that’s a myth. These substances have active compounds that interact just like pharmaceuticals.
Why do some people have worse side effects than others?
Genetics, age, liver and kidney function, and even diet matter. Someone with poor liver function may process drugs slower, leading to buildup. Older adults often have reduced kidney clearance, making side effects more likely. People with CYP2D6 or CYP2C19 gene variants may turn a normal dose into a toxic one. Even something as simple as eating a grapefruit daily can make a drug 300% more potent. What’s safe for one person could be dangerous for another.
Can I trust my pharmacist to catch all interactions?
Pharmacists are trained to check for interactions, but they rely on the information you give them. If you don’t mention your supplements, herbal teas, or over-the-counter meds, they can’t warn you. Also, many pharmacies use automated systems that miss complex or rare interactions. The best defense is you - bring your full list, ask questions, and don’t assume someone else is watching out for you.
What should I do if I think I’m having a drug interaction?
Stop taking the new medication or supplement immediately - but don’t quit your prescription without talking to your doctor. Write down your symptoms: when they started, what you took, and how you feel. Call your doctor or pharmacist. If symptoms are severe - chest pain, confusion, uncontrolled bleeding, or trouble breathing - go to the ER. Bring your medication list. Don’t wait. Many interactions can be reversed if caught early.
Final Thought: Your List Is Your Shield
Medications save lives. But when they interact, they can hurt - sometimes fatally. The good news? Almost half of these reactions are preventable. You don’t need a medical degree to stop them. You just need to know what you’re taking - and speak up.

Comments (8)
vikas kumar
November 25, 2025 AT 23:54Been there. Took statins + grapefruit juice for months before I realized why my muscles felt like wet cardboard. Learned the hard way that ‘natural’ doesn’t mean ‘safe.’ Now I check every new pill against my list - even ginger tea. Seriously, folks, your body’s not a blender.
Vanessa Carpenter
November 26, 2025 AT 12:10My grandma took 12 meds. No one ever asked about her turmeric capsules. She ended up in the ER with a bleed. It wasn’t the doctors’ fault - it was the system. We need better communication, not more alerts that no one reads.
Shannon Amos
November 28, 2025 AT 06:21So let me get this straight - the same people who think ‘detox teas’ cure cancer think ‘natural’ supplements won’t kill you? 🤡
Bethany Buckley
November 29, 2025 AT 04:39The cytochrome P450 system isn’t just a metabolic pathway - it’s a biological negotiation between xenobiotics and endogenous homeostasis. When CYP3A4 is inhibited, pharmacokinetic equilibrium collapses into a cascade of unintended pharmacodynamic consequences. The liver doesn’t ‘fight’ - it becomes a compromised gatekeeper. And yet, we treat polypharmacy like a playlist, not a biochemical minefield. We’ve outsourced vigilance to algorithms that can’t parse context, while patients self-diagnose with WebMD and Instagram influencers. This isn’t negligence. It’s epistemic arrogance disguised as convenience.
Bea Rose
November 29, 2025 AT 10:48St. John’s wort + SSRIs = serotonin syndrome. Done. No more explanations needed.
Wendy Edwards
November 29, 2025 AT 11:52i had a friend who took omeprazole and then started a probiotic because ‘it helps digestion’ and ended up with a bad reaction because the med didn’t work right anymore. she was so mad at the doctor but honestly? she never told anyone about the probiotic. we all think ‘it’s just a pill’ or ‘it’s just a tea’ but nooo. your body’s got a whole system going on. please just write it down. like, on paper. or a note. or a sticky. i’m not even mad anymore, just tired.
stephen riyo
November 30, 2025 AT 20:06Wait, wait, wait - so if I take fish oil and warfarin, I could bleed out? But my cousin takes both and she’s fine? What if I just take less fish oil? Or maybe I just skip the grapefruit? Like… how do I even know what’s dangerous? I don’t have a PhD in pharmacology! Can’t someone just… make a simple chart? Or an app? I mean, I’m not asking for much - just a list that says ‘DON’T MIX THESE’ with emojis? 🚫💊🍇
Michael Collier
December 2, 2025 AT 02:41Thank you for this comprehensive and clinically grounded exposition. The systemic failures in medication reconciliation are not merely administrative oversights - they represent a critical gap in patient safety infrastructure. I would respectfully propose that healthcare institutions implement mandatory, structured medication reconciliation at every point of care transition, supported by AI-driven decision aids that prioritize high-risk interactions based on real-time patient data, including supplement use and dietary patterns. Furthermore, standardized patient education materials - delivered in multiple modalities - should be co-developed with pharmacists and patient advocates to ensure accessibility and comprehension. This is not a call for increased burden on clinicians; it is a call for intelligent, human-centered system redesign.