St. John’s Wort might seem like a harmless natural fix for low mood. You see it on store shelves next to vitamins, labeled "natural mood support" or "herbal antidepressant." But here’s the truth: this plant doesn’t just lift your spirits-it can shut down life-saving medications. If you’re taking anything from birth control to heart drugs to antidepressants, St. John’s Wort could be silently making them useless-or worse, dangerous.
How St. John’s Wort Messes With Your Meds
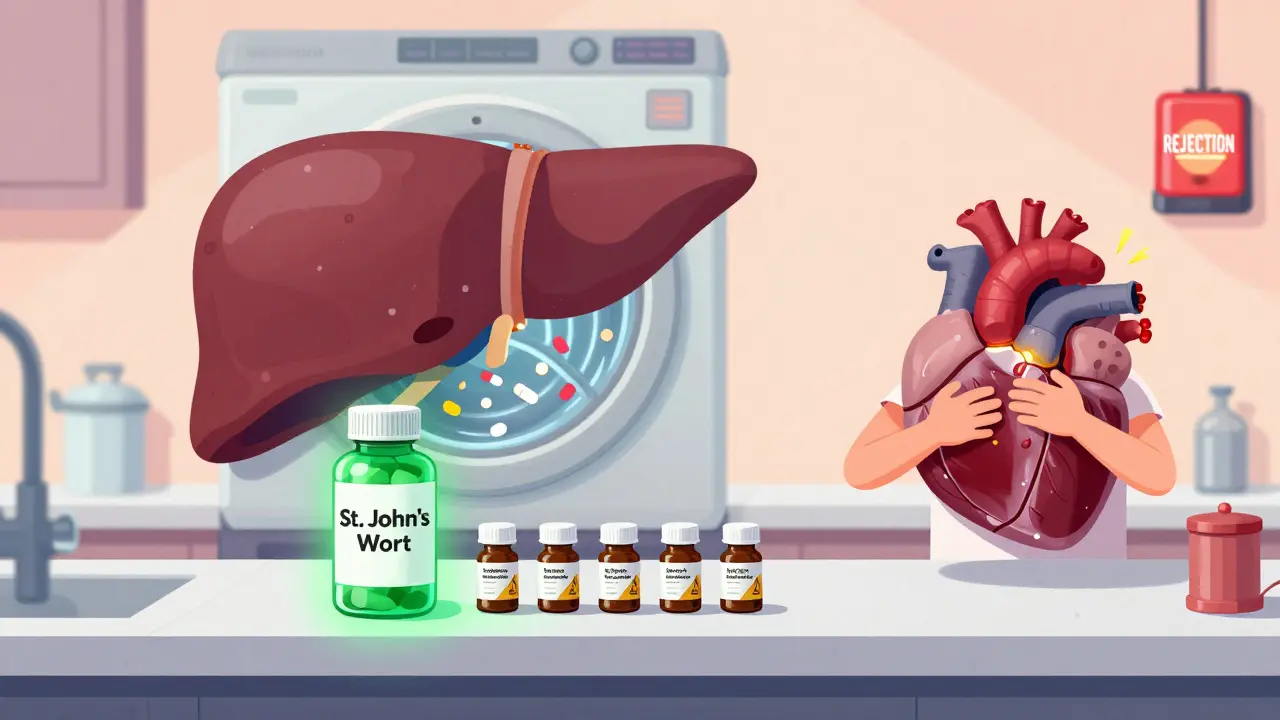
St. John’s Wort doesn’t work like a typical supplement. It’s more like a hidden switch in your body that flips on enzymes that break down drugs too fast. The main culprit? hyperforin is the active compound in St. John’s Wort that turns on the pregnane-X-receptor (PXR), which then cranks up production of liver enzymes CYP3A4, CYP2C9, and CYP1A2. These enzymes are your body’s built-in drug cleaners. When they’re overworked, your medications get flushed out before they can do their job.
Think of it like this: if you’re on a drug that needs to stay in your system at a steady level-say, cyclosporine after a transplant-St. John’s Wort turns your liver into a high-speed washing machine. The result? Drug levels crash. In documented cases, heart transplant patients on cyclosporine had organ rejection because St. John’s Wort dropped their drug levels by over 50%. The same thing happened with kidney transplant patients on tacrolimus. One 2019 report showed a woman’s tacrolimus level fell from 12 ng/mL to 3 ng/mL in under two weeks after starting St. John’s Wort. That’s not just ineffective-it’s life-threatening.
The 12 Medication Categories That Can’t Mix With St. John’s Wort
St. John’s Wort doesn’t play favorites. It messes with a long list of critical drugs. Here are the ones you absolutely need to avoid if you’re considering this herb:
- Immunosuppressants like cyclosporine, tacrolimus, and sirolimus-used after organ transplants. Without these drugs, your body attacks the new organ.
- Antiretrovirals for HIV, including protease inhibitors and non-nucleoside reverse transcriptase inhibitors. Dropping these levels can lead to drug-resistant HIV.
- Oral contraceptives. There are real stories of women getting pregnant while on birth control pills and taking St. John’s Wort. The European Medicines Agency requires this warning on every product sold in the EU.
- Anticoagulants like warfarin. One patient’s INR (a blood-clotting measure) dropped from 2.5 to 1.4 in 10 days after starting St. John’s Wort. That’s a 44% drop in blood-thinning effect-enough to trigger a stroke.
- Antidepressants like SSRIs (Prozac, Zoloft) and SNRIs (Effexor). Combining them can cause serotonin syndrome: agitation, racing heart, high fever, seizures. It’s rare, but deadly.
- Opioid painkillers like oxycodone, methadone, and tramadol. St. John’s Wort can slash their pain-relieving power by up to 70%.
- Statins like atorvastatin and simvastatin. Lowered levels mean higher cholesterol and increased heart attack risk.
- Beta-blockers like metoprolol. Reduced effectiveness can lead to uncontrolled blood pressure or heart rate.
- Calcium channel blockers like amlodipine. Can lead to dangerous spikes in blood pressure.
- Chemotherapy drugs like irinotecan and etoposide. Reduced drug levels mean cancer treatment fails.
- Antifungals like itraconazole. Can lead to fungal infections that don’t respond to treatment.
- Anti-seizure drugs like carbamazepine. May increase seizure frequency.
That’s 12 major categories. The FDA and European Medicines Agency both list over 50 specific drugs with confirmed interactions. The Mayo Clinic says combining St. John’s Wort with antidepressants "might raise the risk of a buildup of high serotonin levels in the body." The Merck Manual warns it "may reduce the effectiveness of oxycodone, methadone, and tramadol." This isn’t a guess. It’s been proven in hospitals.
Why This Isn’t Just a "Natural" Problem
Many people think "natural" means "safe." But St. John’s Wort is more dangerous than many prescription drugs because it’s unregulated. In the U.S., the FDA doesn’t test herbal supplements before they hit shelves. There’s no standardization. One bottle might have 2% hyperforin; another might have 5%. The dose you take matters-but you have no way of knowing.
Compare that to prescription drugs. A pill of fluoxetine (Prozac) has exactly 20 mg of active ingredient. Every time. St. John’s Wort? A 300 mg tablet could contain anywhere from 0.1% to 5% hyperforin. That’s a 50-fold difference in interaction potential. And because it’s sold as a supplement, most people never tell their doctor they’re taking it. A 2017 study found that 68% of patients on immunosuppressants who used St. John’s Wort didn’t mention it to their transplant team.

What About Other Herbal Mood Boosters?
You might wonder: "What about SAM-e or 5-HTP? Are they safer?"
SAM-e has almost no documented interactions-just a small risk if mixed with MAO inhibitors. 5-HTP might slightly increase serotonin, but it doesn’t trigger enzyme induction like St. John’s Wort. Neither affects CYP3A4 or P-glycoprotein. That’s why experts say St. John’s Wort has over 50 major interactions, while SAM-e has maybe two.
And here’s the kicker: St. John’s Wort is the only herbal supplement that’s been shown to interact with drugs as strongly as rifampin-a powerful prescription antibiotic known for causing dangerous interactions. The difference? Rifampin is prescribed with warnings. St. John’s Wort is sold on Amazon with a tiny label saying "may interact with medications."
What Should You Do If You’re Already Taking It?
If you’re on any prescription medication and currently taking St. John’s Wort, don’t stop cold turkey. Here’s what to do:
- Check your meds. Look at every pill you take daily. Even OTC drugs like ibuprofen or antihistamines can be affected.
- Call your pharmacist. Pharmacists have access to interaction databases that doctors don’t always use. Ask them to run a full check on St. John’s Wort and every drug you take.
- Don’t quit abruptly. If you’re using it for depression, stopping suddenly can cause withdrawal symptoms like anxiety, dizziness, or irritability. Work with your doctor to taper off.
- Wait two weeks. The enzyme-inducing effects of St. John’s Wort last up to 14 days after you stop taking it. So even if you quit today, your body is still clearing it out. Don’t start a new medication until that window has passed.
- Ask about alternatives. If you need an herbal option, SAM-e is a safer bet. If you need a real antidepressant, SSRIs like sertraline have no known interaction with herbal supplements.

Who’s Most at Risk?
Women aged 35 to 54 are the biggest users of St. John’s Wort-38% of all users, according to CDC data. That’s likely because they’re more likely to seek natural remedies for depression and anxiety. But they’re also more likely to be on birth control, antidepressants, or thyroid meds. That’s a perfect storm.
Older adults are less likely to use it-only 1.9% of adults over 65 take it. Why? Because they’re usually on 5 or more medications. They’ve already seen what happens when herbs mix with drugs. They know better.
Transplant patients? They’re at the highest risk. One study found that 1 in 4 transplant recipients who took St. John’s Wort had their drug levels drop below the critical threshold within 3 weeks. That’s not a coincidence. That’s a pattern.
The Future of St. John’s Wort
Researchers are trying to fix this. A 2022 study created a low-hyperforin version of St. John’s Wort that cut CYP3A4 induction by 90%. It’s promising-but not yet available. And even if it were, most products on the market today still contain the full, dangerous dose.
Global sales of St. John’s Wort have dropped 37% since 2000. Germany, where it’s prescribed like a drug, still accounts for over 30% of sales. But in the U.S., awareness is growing. The FDA issued new guidance in March 2023 calling St. John’s Wort a "high-risk supplement." That’s a big deal.
The bottom line? St. John’s Wort isn’t harmless. It’s a powerful biochemical tool that can sabotage your health. It’s not the herb’s fault-it’s the lack of regulation and awareness. If you’re taking any prescription medication, don’t risk it. Talk to your pharmacist. Ask for safer alternatives. Your life might depend on it.
Can St. John’s Wort make birth control fail?
Yes. Multiple documented cases show women becoming pregnant while on birth control pills and taking St. John’s Wort. The herb reduces the levels of estrogen and progestin in the bloodstream by triggering liver enzymes that break them down. The European Medicines Agency requires this warning on all products sold in the EU. If you’re using hormonal birth control, avoid St. John’s Wort completely.
How long does it take for St. John’s Wort to start interacting with drugs?
The enzyme-inducing effects begin within 5-7 days, peak around 10-14 days, and can last up to 2 weeks after you stop taking it. That means even if you quit the herb, your medications may still be affected for over two weeks. Don’t assume a short break is safe.
Is St. John’s Wort safer than antidepressants?
It can be-for people who aren’t on other medications. Studies show it works as well as some SSRIs for mild to moderate depression. But if you’re taking any other drug-especially immunosuppressants, anticoagulants, or HIV meds-the risks far outweigh the benefits. The same 2006 study that first linked it to transplant rejection concluded: "The risk-benefit ratio of St. John’s wort is unfavorable when patients are taking concomitant medication."
Can I take St. John’s Wort if I’m on a statin?
No. St. John’s Wort reduces levels of atorvastatin, simvastatin, and lovastatin by up to 60%. This can cause cholesterol to spike, increasing your risk of heart attack or stroke. Even if your cholesterol looked fine before, this interaction can undo months of progress. Talk to your doctor about switching to a statin that doesn’t interact, like pravastatin or rosuvastatin.
Why don’t more people know about this?
Because supplements aren’t required to list interactions on labels in the U.S. The FDA only requires a general disclaimer: "This product is not intended to diagnose, treat, cure, or prevent any disease." Most people assume that means it’s safe. But the FDA issued a Public Health Advisory in 2000 warning about these interactions. The problem isn’t lack of evidence-it’s lack of enforcement.
What should I do if I think St. John’s Wort is affecting my medication?
Stop taking it immediately and contact your doctor or pharmacist. If you’re on a drug with a narrow therapeutic index-like warfarin, cyclosporine, or tacrolimus-ask for a blood test to check your drug levels. Symptoms like increased anxiety, breakthrough bleeding (if on birth control), or unexplained pain (if on opioids) could be signs of reduced drug effectiveness. Don’t wait.

Comments (9)
Joanne Tan
February 11, 2026 AT 14:48omg i just realized i’ve been taking this with my birth control for months 😳 i thought it was just a ‘natural mood boost’ like they say on the label. no wonder i got pregnant last year. my pharmacist is gonna kill me. thanks for this post, i’m deleting it from my cart right now.
Ojus Save
February 12, 2026 AT 00:19bro i took this for anxiety and now my uncle’s transplant med is acting weird… he’s in the hospital. i had no idea. why is this even sold like candy??
Jason Pascoe
February 13, 2026 AT 06:20There’s something deeply unsettling about how easily we accept ‘natural’ as synonymous with ‘safe.’ St. John’s Wort isn’t some gentle tea-it’s a biochemical sledgehammer that’s been quietly wrecking lives for decades. The fact that it’s sold without standardized dosing, without mandatory interaction warnings, and without any real oversight is a systemic failure. We regulate vitamins like candy but treat real pharmacological agents like folk remedies. It’s not just ignorance-it’s negligence dressed up as freedom.
And yet, here we are, trusting Amazon reviews over peer-reviewed journals. The irony? The same people who scream about Big Pharma are the ones unknowingly poisoning themselves with unregulated herbal cocktails. This isn’t about herbalism. It’s about how we’ve outsourced critical health literacy to marketing departments.
Rob Turner
February 13, 2026 AT 12:51Yeah, I remember when my mate in Sydney started taking this for his low mood after his divorce. He was on warfarin for a clot. One day he came in with a black eye-turns out he’d bruised himself just by bumping into a door. INR dropped to 1.1. He nearly had a stroke. 😳
Pharmacist spotted it before the doctor even did. We all assumed ‘herbal’ = ‘harmless.’ Turns out the herb’s got more teeth than a piranha. Never again. Also, I’ve started calling it ‘The Silent Saboteur.’ Sounds dramatic? Nah. It’s accurate.
Luke Trouten
February 14, 2026 AT 01:30The most troubling aspect of this isn’t even the pharmacology-it’s the cultural blind spot. We’ve built a society where ‘natural’ is a moral virtue, and ‘pharmaceutical’ is a corporate villain. This creates a dangerous cognitive dissonance: people trust the label on a bottle of St. John’s Wort more than the label on their prescribed medication. But the supplement has zero regulatory oversight, while the prescription has undergone decades of clinical trials, batch testing, and post-market surveillance.
It’s not that herbs are inherently bad. It’s that we’ve allowed a market to commodify biochemical complexity without accountability. The real tragedy is that people aren’t being warned-they’re being sold a myth.
Gabriella Adams
February 15, 2026 AT 20:30As someone who works in clinical pharmacy, I see this every single week. A 42-year-old woman comes in with a new prescription for sertraline-then casually mentions she’s been taking St. John’s Wort for ‘a little extra help.’ I ask how long. She says, ‘Since last summer.’
By then, her sertraline levels are practically undetectable. She thinks she’s not responding to treatment. She’s not. The herb wiped it out.
We don’t have a ‘natural remedies’ problem-we have a ‘we don’t talk to our providers’ problem. If you’re taking anything herbal and you’re on meds? Tell your pharmacist. Even if you think it’s ‘just a little.’ It’s not.
Kristin Jarecki
February 17, 2026 AT 06:10Thank you for this meticulously detailed and clinically accurate breakdown. I wish every pharmacy in the U.S. had a mandatory screening protocol for herbal supplement use before dispensing high-risk medications. The FDA’s 2023 guidance is a step forward, but enforcement remains toothless. We need labeling standards as rigorous as those for prescription drugs: clear, visible, and non-negotiable.
Also, I appreciate the distinction between St. John’s Wort and SAM-e or 5-HTP. Not all botanicals are created equal, and we must stop conflating them. The problem isn’t herbal medicine-it’s unregulated, unstandardized, and poorly understood botanicals with potent pharmacokinetic effects.
Ernie Simsek
February 18, 2026 AT 19:17LMAO imagine being so dumb you take a plant that’s basically a drug-melting laser and then wonder why your antidepressant stopped working 😂
My cousin’s mom took this with her blood thinner and ended up in the ER with a pulmonary embolism. She thought it was ‘just a mood booster.’ Bro, it’s a biochemical grenade. Stop being naive.
Stacie Willhite
February 20, 2026 AT 17:46I’m so glad someone finally put this out there. I’ve been a nurse for 12 years and I’ve seen too many patients come in with ‘I didn’t think it mattered’-and then it did. I always ask about supplements, but most people don’t even think of them as ‘meds.’
If you’re reading this and you’re on any prescription, please, just pause. Check with your pharmacist. It takes five minutes. It could save your life.