Every year, thousands of patients in the U.S. are harmed or die because of mistakes in how their medicines are dispensed. Not because pharmacists are careless. Not because nurses are sloppy. But because the systems they work in are flawed. The patient safety goals set by The Joint Commission aren’t optional checklists-they’re the bare minimum needed to stop preventable harm. And in 2026, those standards are more critical than ever.
Why Medication Errors Still Happen
You’d think with all the technology we have, prescribing and dispensing errors would be rare. But they’re not. According to the Agency for Healthcare Research and Quality, one in every 131 outpatient deaths and one in every 8,548 inpatient deaths are tied to medication errors. That’s not a statistic-it’s a system failure. The old idea of the “Five Rights” (right patient, right drug, right dose, right route, right time) sounds solid. But here’s the truth: 83% of errors happen even when all five rights are confirmed. Why? Because relying on a person to remember and verify everything during a 12-hour shift with 10 patients is unrealistic. It’s like asking a chef to cook 20 meals at once without a recipe, timer, or labeled ingredients. The real problem isn’t human error-it’s poor system design. A nurse might scan a barcode, but if the automated dispensing cabinet lets her override the alert for a “stat” order, the system is broken. A pharmacist might label a syringe, but if the label is too small or missing the concentration, the next person won’t see the danger.The Joint Commission’s 2025 Patient Safety Goals
The National Patient Safety Goals (NPSGs) are updated every year by The Joint Commission, the group that accredits 96% of U.S. hospitals. In 2025, they sharpened their focus on medication safety with three major updates:- NPSG.03.04.01: Label everything. Every container-syringe, IV bag, cup, vial-must have a label with the drug name, strength, and concentration. The font size? Minimum 10-point. No exceptions. In operating rooms, unlabeled syringes are still found in 27% of facilities. That’s not negligence. It’s systemic neglect.
- NPSG.03.05.01: Anticoagulants are deadly if mismanaged. Warfarin, heparin, direct oral anticoagulants-these drugs have narrow safety margins. The goal? 95% of patients on these meds must have documented INR levels, clear therapeutic ranges, and patient education. No guessing. No shortcuts.
- New requirement: Bedside specimen labeling. Labels on blood tubes must be applied in front of the patient using two identifiers (name and DOB). Why? Mislabeling leads to 160,000 adverse events a year. That’s not a typo. That’s 160,000 people getting the wrong diagnosis because someone labeled a tube in the hallway.
High-Alert Medications: The Silent Killers
Some drugs are so dangerous that even a small mistake can kill. These are called high-alert medications. Insulin, opioids, concentrated potassium chloride, and injectable promethazine are on that list. Promethazine? You might not know it, but between 2006 and 2018, it caused 37 amputations because it was accidentally injected into an artery instead of a vein. The tissue around the injection site dies. The limb is lost. All because a nurse grabbed the wrong vial, or didn’t double-check the label. The Institute for Safe Medication Practices (ISMP) says the fix isn’t just training-it’s system control. That means:- Storing high-alert meds in separate, locked bins
- Using barcode scanning at every step-from the pharmacy shelf to the bedside
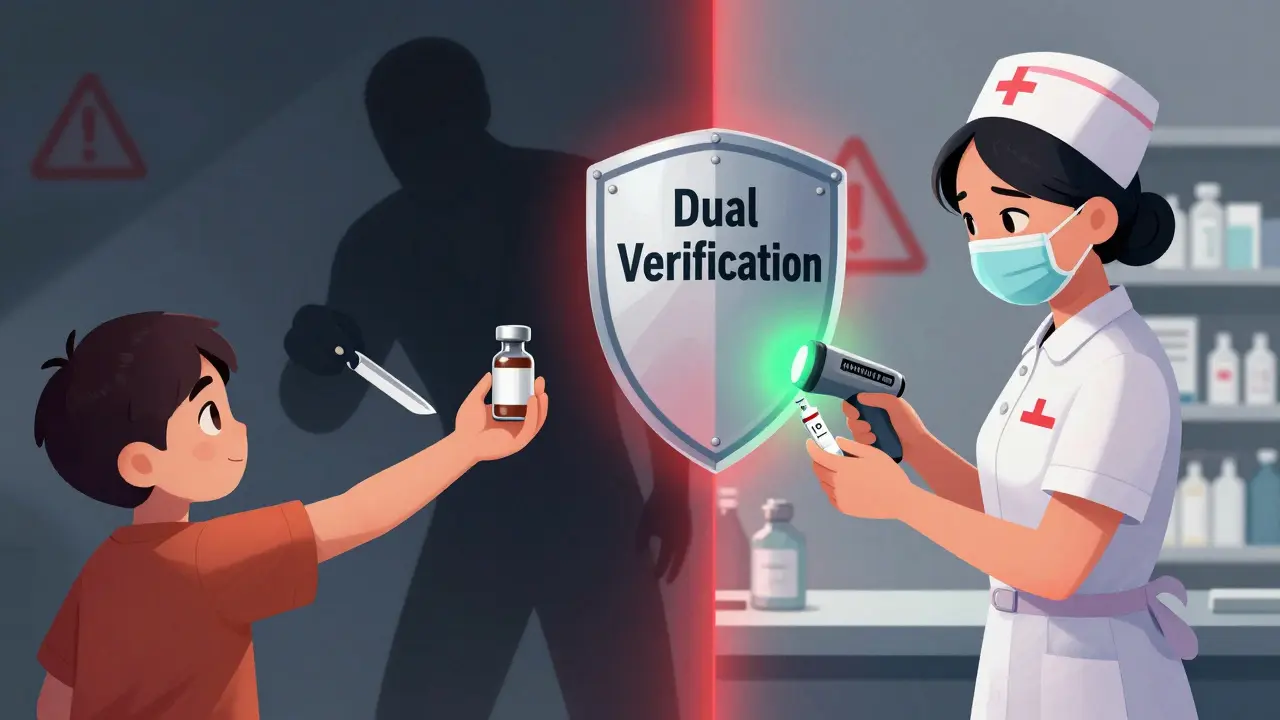
- Requiring two licensed staff to verify high-risk doses before administration
Technology Isn’t the Fix-It’s the Tool
Barcodes, automated dispensing cabinets (ADCs), and electronic health records sound like magic bullets. And they are-if used right. One hospital reduced wrong-drug errors by 86% after implementing barcode medication administration. But guess what? Nurses spent 7.2 extra minutes per dose scanning barcodes. That’s 72 extra minutes per shift for a nurse with 10 patients. The result? Staff burnout. The solution? Hire more staff. Or redesign workflows. Automated dispensing cabinets are supposed to prevent errors. But when pharmacists report override rates above 5%, those cabinets become the problem. Why? Emergency orders. Staff shortcuts. Lack of training. In one study, facilities with override rates over 5% had 3.7 times more medication errors. The tech doesn’t fail. People bypass it. And if you don’t audit those bypasses, you’re just pretending to be safe.What Works: Real Stories from the Front Lines
The Children’s Hospital of Philadelphia didn’t just update their policy. They rebuilt their entire pediatric medication system. Here’s what they did:- Weight-based dosing protocols with built-in alerts in the EHR
- Double-checks for all high-alert meds in NICU and PICU
- Pharmacists embedded in pediatric units, not just working behind the counter

The Hidden Cost of Skipping Safety
It’s easy to think safety is expensive. But the real cost is in the damage. The Centers for Medicare & Medicaid Services now tie 2% of hospital reimbursements to patient safety outcomes. Miss your targets, and you lose money. But more importantly, you lose trust. Pharmacists who skip labeling, skip scanning, or skip double-checks aren’t just breaking rules-they’re gambling with lives. And the data doesn’t lie: facilities with strong safety cultures and executive sponsorship have an 89% chance of sustaining their programs for five years. Those without? Only 42% make it.What You Can Do Right Now
You don’t need a $2 million software upgrade to start improving safety. Here’s how to begin:- Audit your labeling. Walk into your pharmacy and check 10 random vials or syringes. Do they have the drug name, strength, and concentration? Is the font readable from 2 feet away?
- Track your ADC overrides. How many times did staff bypass the system last week? If it’s more than 5%, investigate why. Is it because the system is slow? Or because staff feel pressured to move fast?
- Start a weekly safety huddle. Every Monday, spend 15 minutes with your team reviewing near-misses. Not to blame. To learn. “What almost went wrong? What could we change?”
- Push for dual verification on high-alert meds. Even if your policy doesn’t require it, do it anyway. One extra check saves lives.
- Train your staff on the 2025 NPSGs. Don’t assume they know them. Test them. Ask: “What’s required on a medication label?” “What’s the target INR range for warfarin?”
The Future Is Here
Artificial intelligence is starting to help. Mayo Clinic’s pilot program used AI to predict which patients were at risk for adverse drug events. It cut potential harm by 47%. That’s not science fiction. That’s now. The World Health Organization wants every country to adopt these standards by 2030. But right now, only 22% of low- and middle-income countries have them. The truth? Patient safety isn’t about technology. It’s about culture. It’s about leaders who care enough to fund training, not just buy machines. It’s about pharmacists who refuse to accept “that’s how we’ve always done it.” In 2026, the goal isn’t to be perfect. It’s to be better than yesterday. And that starts with one label. One scan. One double-check.What are the current Joint Commission medication safety goals for 2026?
The 2025 National Patient Safety Goals (NPSGs), which remain in effect into 2026, require healthcare facilities to label all medications with drug name, strength, and concentration using a minimum 10-point font; implement standardized practices for anticoagulant therapy including INR monitoring and patient education; and apply bedside specimen labels using two patient identifiers. New emphasis is placed on managing automated dispensing cabinet overrides and preventing errors with high-alert medications like insulin, opioids, and injectable promethazine.
Why is the Five Rights rule not enough to prevent medication errors?
The Five Rights-right patient, drug, dose, route, and time-are a checklist, not a system. Studies show 83% of medication errors happen even when all five rights are confirmed. This is because the model places the burden on individuals during high-stress, high-volume conditions. Without system safeguards like barcode scanning, double-checks, and smart technology, human memory and attention fail. The solution isn’t better training alone-it’s better design.
What are high-alert medications and why do they need special handling?
High-alert medications have a high risk of causing serious harm if used incorrectly. Examples include insulin, opioids, concentrated potassium chloride, and injectable promethazine. Even small errors-wrong dose, wrong route, wrong patient-can lead to death or permanent injury. Special handling includes separate storage, mandatory dual verification, barcode scanning, and restricted access. For example, promethazine injections caused 37 amputations between 2006 and 2018 because they were accidentally given into arteries instead of veins.
How do automated dispensing cabinets contribute to medication errors?
Automated dispensing cabinets (ADCs) are designed to reduce errors by controlling access and tracking usage. But when staff override safety alerts-often for urgent or stat orders-the risk increases. Facilities with override rates above 5% have 3.7 times more medication errors. Overriding isn’t always malicious; it’s often due to poor workflow design, lack of training, or time pressure. The fix isn’t banning overrides-it’s reducing the need for them through better inventory management and staff support.
What’s the difference between Joint Commission NPSGs and ISMP best practices?
The Joint Commission’s NPSGs are mandatory standards for accredited hospitals. They’re the legal baseline. The Institute for Safe Medication Practices (ISMP) best practices are voluntary guidelines developed by pharmacists and safety experts. They’re more detailed and proactive-covering 25 specific high-risk scenarios by 2026. While 96% of U.S. hospitals follow NPSGs, only 68% adopt ISMP practices. But hospitals that use both see the lowest error rates.
Can technology like AI really reduce medication errors?
Yes. Pilot programs at Mayo Clinic and other leading hospitals use AI to analyze patient data and predict potential adverse drug events before they happen. One program reduced potential harm by 47% by flagging risky combinations, duplicate orders, or incorrect dosing based on weight or kidney function. AI doesn’t replace pharmacists-it gives them real-time intelligence to catch errors humans might miss during busy shifts.
How can a pharmacy start improving safety without a big budget?
Start small and focus on culture. Audit your labeling practices. Track how often staff override automated systems. Hold a 15-minute weekly safety huddle to review near-misses without blame. Require dual verification for high-alert drugs-even if it’s not policy. Train staff on the 2025 NPSGs. Use free tools from ECRI Institute to self-assess. Real change doesn’t come from expensive software. It comes from people deciding they won’t accept avoidable harm anymore.


Comments (9)
Kiran Plaha
January 6, 2026 AT 10:58Man, I’ve seen this in India too-nurses skipping labels because they’re swamped. No fancy tech, just people trying to survive shifts. But the 10-point font rule? That’s basic. Why are we still arguing about this?
Matt Beck
January 7, 2026 AT 17:45Okay, but let’s be real 🤔-we’re treating pharmacy like it’s a video game where you level up by not killing patients. 😅 The Five Rights? More like Five Suggestions. We need systems that don’t rely on humans being perfect. 🧠💊 #PharmLife
Ryan Barr
January 8, 2026 AT 13:56Labeling. Dual checks. Barcodes. These aren’t innovations. They’re hygiene. If your hospital needs a blog post to understand this, you shouldn’t be dispensing.
Cam Jane
January 9, 2026 AT 03:32Y’all, I work in a small community pharmacy and we started doing weekly safety huddles last month. Just 15 minutes. No blame. Just ‘what almost went wrong?’ We caught a mislabeled insulin vial because someone said, ‘Wait, that label looks weird.’ No one got hurt. That’s the win. You don’t need a $2M system-you need a team that talks. And listens. And cares enough to pause. 💪❤️
Dana Termini
January 10, 2026 AT 16:21I get the frustration with overrides and burnout. But I also see pharmacists who feel like they’re the only ones fighting for safety. We need leadership to back this up-not just policies, but time, staffing, real support. It’s not about being perfect. It’s about being human.
Wesley Pereira
January 12, 2026 AT 13:08So let me get this straight… we spend billions on EHRs but still let nurses override alerts because ‘it’s stat’? Classic. 🤦♂️ And now we’re surprised when people get amputated from promethazine? Bro. It’s not a glitch. It’s a culture of ‘move fast and break things’… except here, people are the things breaking.
Isaac Jules
January 13, 2026 AT 18:18Anyone who thinks this is just about ‘training’ is delusional. You can’t train out a broken system. You can’t ‘motivate’ your way out of 12-hour shifts with zero support. This isn’t a ‘what you can do’ article-it’s a cry for systemic collapse. And we’re all just cleaning up the mess while pretending we’re heroes.
Amy Le
January 15, 2026 AT 10:03America’s healthcare system is a joke. We spend more than any country on earth, and still let people die because someone didn’t use a 10-point font? Meanwhile, other countries have universal care and zero promethazine amputations. We don’t need better guidelines-we need to stop pretending capitalism fixes everything.
Pavan Vora
January 16, 2026 AT 14:43From India-where we dont have barcode scanners or ADCs-we still make labels by hand with big letters. Why? Because we saw a kid get the wrong dose. No tech. Just care. Maybe the answer isn’t more gadgets… but more respect for the person holding the syringe.