Orthostatic Hypotension Medication Risk Calculator
How Much Risk Do You Have?
This tool calculates your risk of orthostatic hypotension based on medications you're taking and your age. The risk increases with age and multiple medications.
Standing up too fast and feeling like the room is spinning? That dizzy spell isn’t just bad luck-it could be your medications. Orthostatic hypotension, or orthostatic hypotension, is when your blood pressure drops suddenly as you rise from sitting or lying down. This causes reduced blood flow to your brain, leading to lightheadedness, blurred vision, or even fainting. It’s not rare. In people over 70, up to 30% experience it. And in many cases, it’s not aging alone-it’s the drugs they’re taking.
What Exactly Happens When You Stand Up?
When you stand, gravity pulls blood down into your legs. Normally, your body reacts instantly: your heart beats faster, your blood vessels tighten, and your blood pressure stays steady so your brain keeps getting oxygen. But if that system is messed up, your pressure plummets. The medical definition is clear: a drop of more than 20 mm Hg in systolic pressure or 10 mm Hg in diastolic pressure within three minutes of standing. And if you feel dizzy, lightheaded, or faint at the same time? That’s orthostatic hypotension.It’s not just about getting up too fast. It’s about what’s happening inside your body-and often, that’s linked to the pills you’ve been prescribed.
Which Medications Cause This?
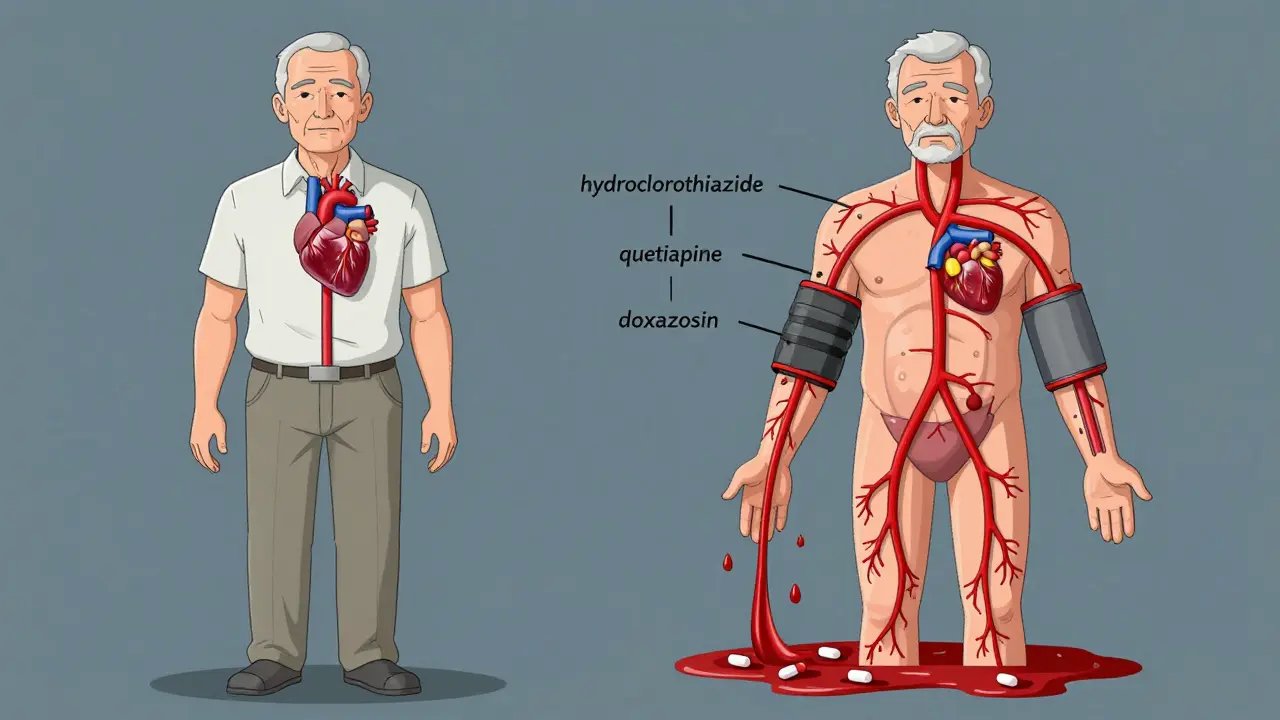
Some drugs are notorious for triggering this drop in blood pressure. The most common culprits fall into a few key groups:- Antihypertensives-drugs meant to lower blood pressure can lower it too much. Diuretics like hydrochlorothiazide, ACE inhibitors like lisinopril, and calcium channel blockers are frequent offenders. They reduce fluid volume or relax blood vessels, making it harder to maintain pressure when standing.
- Antidepressants-especially tricyclics like amitriptyline. These block norepinephrine, a chemical your body needs to tighten blood vessels. Studies show they increase OH risk by over 3 times.
- Alpha-blockers-used for prostate issues or high blood pressure. Drugs like doxazosin and terazosin directly prevent blood vessels from constricting. Their OH risk is nearly 3 times higher than other BP meds.
- Antipsychotics-clozapine, quetiapine, and chlorpromazine are big ones. They affect brain signals that control blood pressure. Up to 40% of people on high doses report dizziness on standing.
- Opioids-morphine, oxycodone, and hydrocodone can depress the nervous system. About 1 in 5 elderly patients on opioids get OH. The risk jumps even higher if they’re also taking benzodiazepines or drinking alcohol.
- Levodopa-used for Parkinson’s, this drug can cause OH in up to half of users. The body struggles to adjust blood pressure as movement changes.
It’s not just the drug itself-it’s the combo. Someone on five medications has nearly 6 times the risk of someone on one or two. Polypharmacy isn’t just a buzzword-it’s a real danger.
Why Older Adults Are More at Risk
Age isn’t just a number here. As you get older, your body’s ability to regulate blood pressure slows down. Baroreceptors-your body’s pressure sensors-become less sensitive. Blood vessels stiffen. The heart doesn’t respond as quickly. All of this makes you more vulnerable.But add medications to that? The risk skyrockets. People over 70 are 3.2 times more likely to develop orthostatic hypotension than younger adults. And if you’re taking four or more medications? Your risk jumps to 5.7 times higher. That’s not a small increase-it’s a major red flag.
Many older adults don’t realize their dizziness isn’t normal. They think it’s just getting older. But this isn’t just annoying-it’s dangerous. About 15% to 30% of people with OH fall at least once a year. Falls lead to fractures, hospital stays, and even death. Studies show a 24% to 32% higher risk of dying over 10 years if you have untreated orthostatic hypotension.
How Doctors Diagnose It
It’s not a guess. Diagnosis is based on numbers. Your doctor should measure your blood pressure while you’re lying down for at least five minutes, then again after you stand up-at one, two, and three minutes. The drop has to meet the >20/>10 mm Hg threshold. Symptoms must match the timing too.But here’s the problem: many patients don’t report dizziness. Up to 40% of people with orthostatic hypotension have no symptoms. They’re just more likely to fall. That’s why screening is critical, especially for those on high-risk meds.
Since 2022, the American Geriatrics Society’s Beers Criteria has listed 12 medications that should be avoided or used with extreme caution in older adults because of OH risk. Many U.S. clinics now screen patients over 65 during routine visits. If you’re on any of those meds and feel dizzy when standing, ask for a BP check.
What You Can Do About It
The good news? Medication-induced orthostatic hypotension is often reversible. In 65% to 80% of cases, symptoms improve once the cause is addressed.Here’s what works:
- Review your meds-Don’t assume all your prescriptions are necessary. Ask your doctor: "Which of these could be causing my dizziness?" Sometimes, switching to a different drug in the same class helps. For example, ziprasidone causes far less OH than clozapine. Or replacing hydrochlorothiazide with a different diuretic might make a difference.
- Stand up slowly-Wait a few seconds after sitting up before standing. Sit on the edge of the bed for 30 seconds. Use your arms to push up. Don’t rush.
- Stay hydrated-Drink 2 to 2.5 liters of water a day. Fluids help maintain blood volume. Dehydration makes OH worse.
- Wear compression stockings-These help push blood back up from your legs. They’re simple, cheap, and effective. Studies show they reduce symptoms in over half of users.
- Avoid heat and alcohol-Hot showers, saunas, and alcohol all dilate blood vessels. That’s the last thing you need if you’re already prone to low pressure.
- Elevate the head of your bed-Sleeping with your head slightly raised (6 to 9 inches) helps reduce overnight fluid shifts and improves morning blood pressure.
If those steps don’t help, your doctor might consider medication like midodrine, which tightens blood vessels. It’s not first-line, but it’s effective for those who still struggle after lifestyle changes.

Real Stories, Real Impact
One patient on Reddit, "AnxiousSenior89," started quetiapine for anxiety and fainted twice within three weeks. Her blood pressure dropped from 128/82 to 92/61 in under two minutes. After switching meds, the dizziness vanished. Another case from Cleveland Clinic’s forums: a 78-year-old on six medications had repeated falls. Removing hydrochlorothiazide alone resolved the OH in just 72 hours. But too often, it takes months for doctors to connect the dots. A Mayo Clinic study found 55% of patients had symptoms for over two months before anyone realized it was medication-related. That delay is dangerous.What’s Changing in 2025
The healthcare system is catching up. Since 2020, the FDA requires all new drugs with a 5% or higher OH incidence to include warnings in their labeling. In 2023, the American Heart Association updated its guidelines to recommend midodrine as a first-line treatment when non-drug options fail. Research is also moving toward personalized medicine. Clinical trials are testing genetic markers to predict who’s more likely to develop OH from certain drugs. Soon, doctors might be able to avoid high-risk meds before they’re even prescribed.For now, the best defense is awareness. If you’re over 65, on multiple medications, and feel dizzy when you stand up-don’t ignore it. Don’t assume it’s just part of aging. Ask your doctor to check your blood pressure standing up. Bring your full med list. And if you’re not getting answers, ask again. This is preventable. And it’s life-changing.
Can orthostatic hypotension go away on its own?
Yes, if it’s caused by medication. In 70% to 85% of cases, symptoms improve or disappear after adjusting, reducing, or stopping the drug. But if it’s caused by nerve damage from diabetes or Parkinson’s, it’s less likely to resolve without treatment. The key is identifying the cause. Medication-induced OH is often reversible; neurogenic OH is not.
Is dizziness when standing always orthostatic hypotension?
No. Other causes include inner ear problems, dehydration, low blood sugar, heart rhythm issues, or anxiety. But if the dizziness happens only when standing and improves when sitting or lying down, orthostatic hypotension is likely. A simple blood pressure check while lying and standing can confirm it. Don’t assume it’s something else-get it checked.
Which is worse: orthostatic hypotension from meds or from Parkinson’s?
Both are serious, but medication-induced OH is easier to fix. With drug-related OH, symptoms often improve within days or weeks of stopping or switching the medication. In Parkinson’s, the nerve damage is permanent, so the body can’t regulate pressure properly. Treatment focuses on managing symptoms, not curing the cause. That’s why avoiding high-risk meds in the first place is so important.
Can I just stop taking my blood pressure pill if I feel dizzy?
No. Never stop or change a prescribed medication without talking to your doctor. Stopping suddenly can cause dangerous spikes in blood pressure or make your original condition worse. Instead, report your symptoms. Your doctor can adjust the dose, switch to a different drug, or add a non-drug strategy like compression stockings. The goal is safety-not stopping meds altogether.
How often should I get my blood pressure checked if I’m on high-risk meds?
If you’re over 65 and taking any of the high-risk medications-like diuretics, alpha-blockers, or antipsychotics-you should have your standing blood pressure checked at least once a year. If you’re newly started on one of these drugs, get checked within the first two weeks. If you feel dizzy, get checked right away. Many doctors skip this step, so be proactive. Bring a home BP monitor if you have one.
What to Do Next
If you or someone you care about is feeling dizzy when standing:- Write down every medication, supplement, and over-the-counter pill you take.
- Track when dizziness happens-after standing? After meals? After taking a pill?
- Ask your doctor to check your blood pressure lying down and standing up during your next visit.
- Ask: "Could any of these meds be causing my dizziness? Is there a safer alternative?"
- Start drinking more water and avoid sudden movements.
This isn’t something to brush off. It’s a warning sign your body is under stress. But with the right steps, it’s also something you can fix-without giving up the treatments you need.


Comments (12)
Bradly Draper
December 29, 2025 AT 08:48I used to get dizzy every time I stood up after my blood pressure pill. Thought it was just me getting old. Turns out it was the hydrochlorothiazide. My doctor switched me to a different one and boom-no more spinning rooms. Took me six months to speak up though. Don’t wait like I did.
Just say something. Your body’s trying to tell you something.
Gran Badshah
December 29, 2025 AT 18:21in india we dont even have proper bp machines in small clinics. my uncle fell and broke hip because no one checked standing bp. he was on 7 meds. doctors just shrug and say 'old age'. no one cares. why do you think we have so many falls in elderly? because no one checks. just give the pill. no follow up. no nothing.
Ellen-Cathryn Nash
December 31, 2025 AT 05:29Oh sweet mercy. Another person who thinks their meds are harmless. Let me guess-you also think ‘natural remedies’ fix everything? You don’t just ‘drink more water’ and call it a day when your nervous system is being sabotaged by a pharmacy’s profit margin.
People die from this. Not ‘oh I got a little dizzy.’ People end up in the ER with cracked skulls because someone thought ‘it’s just aging.’
And yes, I’m talking to you, the person who’s still on that alpha-blocker because ‘it’s fine.’ It’s not fine. It’s a ticking time bomb wrapped in a prescription bottle.
Samantha Hobbs
December 31, 2025 AT 16:11OMG I JUST REALIZED MY MOM DOES THIS. SHE’S ON 5 THINGS AND ALWAYS SAYS ‘I’M JUST GETTING CLUMSY.’ I’M TAKING HER TO THE DOCTOR MONDAY. THANK YOU FOR THIS POST. I’LL BUY HER COMPRESSION STOCKINGS TOO 😭
PS: she drinks wine every night. no wonder.
Nicole Beasley
January 2, 2026 AT 05:25This is so important!! 🙌 I had no idea meds could do this. My grandma used to say ‘I’m just slow’ but now I know she was getting dizzy from her heart med. We’re getting her BP checked next week. Also, compression socks are cute now?? 😍 I’ll get her some with flowers. 💕
sonam gupta
January 2, 2026 AT 12:13why do americans need so many pills just to stand up. in india we take one or two at most. our elders walk barefoot in morning and drink warm water. no dizziness. no problems. you overmedicate everything. your system is broken not your body.
Hakim Bachiri
January 2, 2026 AT 23:18Let’s be real-this isn’t about ‘medications.’ It’s about the pharmaceutical-industrial complex. Big Pharma doesn’t want you to know that 80% of these ‘conditions’ are iatrogenic. They profit from your dizziness. They profit from your falls. They profit from your hospital stays.
And don’t get me started on midodrine-$200 a month for a vasoconstrictor that was invented in 1962. Classic. Meanwhile, your doctor is too busy clicking ‘approve’ on the EHR to ask you if you feel like a zombie when you stand up.
And yes, I’ve read the FDA labels. And the Beers Criteria. And the AHA guidelines. I’m not just some guy on Reddit. I’m a *professional* at this. You’re welcome.
Debra Cagwin
January 4, 2026 AT 03:22If you’re reading this and you’re worried about dizziness when standing-you’re already doing better than most. You’re paying attention. That’s huge.
Don’t be afraid to ask your doctor: ‘Could this be my meds?’ Write down your symptoms. Bring your pill bottle. Take a friend. You deserve to feel safe in your own body.
And if your doctor brushes you off? Find another one. Your health isn’t negotiable. You’re not ‘just getting old.’ You’re a person with a right to move without fear. And I’m rooting for you. 💪❤️
Celia McTighe
January 4, 2026 AT 09:30Just had a chat with my 74-year-old neighbor who started quetiapine last year. She said she felt like she was ‘floating through fog’ every morning. We made a pact: every time she stands up, she counts to three. She’s been doing it for two weeks. No more falls. No more panic.
Also, she got compression socks with cats on them. 😻
Small changes. Big impact. You got this. And if you need someone to check in? I’m here. No judgment. Just tea and a listening ear. ☕️
Ryan Touhill
January 4, 2026 AT 13:42Interesting how the article conveniently omits the fact that the FDA’s 2020 labeling requirement was pushed through by activist groups funded by... well, let’s just say the same people who profit from ‘alternative’ BP monitors and ‘natural’ supplements.
And midodrine? A drug that was pulled from the EU market for cardiac risks. But sure, let’s make it ‘first-line’ in the U.S. because why not?
Also, ‘polypharmacy’ is a buzzword. The real issue? Lack of coordinated care. Your PCP prescribes. Your cardiologist prescribes. Your psychiatrist prescribes. No one talks. And you? You’re the one standing there dizzy, holding seven pill bottles.
It’s not the meds. It’s the system. And no, I’m not a conspiracy theorist. I’m a former hospital administrator. I’ve seen the charts.
Teresa Marzo Lostalé
January 6, 2026 AT 04:56There’s a quiet kind of grief in realizing your body doesn’t work the way it used to. Not because you’re broken-but because the tools meant to help you are quietly breaking you instead.
I used to think dizziness was just… part of the deal. Like gray hair. Like forgetting names. But this? This is different. It’s not aging. It’s neglect.
And maybe that’s the real tragedy-not that we’re getting older, but that we’re taught to ignore the signals until it’s too late.
So I stand. Slowly. I drink water. I wear the socks. And I say no-not out of rebellion, but out of reverence. For my body. For my life. For the quiet dignity of standing up without fear.
ANA MARIE VALENZUELA
January 6, 2026 AT 23:17Let’s cut the fluff. If you’re dizzy when you stand, you’re probably on too many meds. Period. You’re not ‘fragile.’ You’re overmedicated. Your doctor is lazy. Or worse-they’re getting paid to keep you on these pills.
Stop drinking water like it’s a cure. Stop buying ‘compression socks’ like they’re fashion. You need a med review. Not a lifestyle hack.
And if your doctor says ‘it’s normal for your age’? Fire them. Find someone who actually reads the Beers Criteria. Or better yet-go to a geriatric pharmacist. They’re the only ones who know what’s really going on.
This isn’t ‘awareness.’ This is damage control. And you’re late to the party.