SSRI Sexual Dysfunction Treatment Pathway Calculator
Your Situation
Recommended Approach
Based on your situation
Best Option:
Success Rate:
Key Considerations:
Sexual side effects from SSRIs aren’t rare-they’re common. If you’re taking an SSRI for depression and notice your libido has dropped, orgasm feels out of reach, or arousal just doesn’t happen like it used to, you’re not alone. Between 35% and 70% of people on these medications experience some form of sexual dysfunction. And it’s not just a minor annoyance. For many, it’s the reason they stop taking their antidepressant altogether. About 1 in 6 people quit their medication because of it.
Why This Happens
SSRIs work by increasing serotonin in the brain. That helps lift mood. But serotonin also plays a role in sexual response. Too much of it can shut down desire, delay orgasm, or make it impossible to get or keep an erection. These effects usually show up within the first few weeks of starting the medication. The problem? Many people don’t know this is a possible side effect until it happens. A 2023 Harvard Health poll found that 73% of patients said their doctor never brought up sexual side effects before prescribing an SSRI.Dose Reduction: Less Is Sometimes More
Before switching medications or adding something new, try lowering the dose. For people with mild to moderate depression, cutting the SSRI dose by 25% to 50% often improves sexual function without making depression worse. Studies show this works for 40% to 60% of users. It’s not a magic fix-some people still struggle-but it’s low-risk and worth trying first. If you’re on 40mg of sertraline, ask your doctor if 20mg or 30mg might still control your mood while giving your sex life back some space.Drug Holidays: Timing It Right
A drug holiday means taking a short break from your SSRI-usually 48 to 72 hours-before planned sexual activity. This works best with SSRIs that leave your system quickly: sertraline, citalopram, escitalopram, and fluvoxamine. For these, stopping for a couple of days can restore normal sexual function. But don’t try this with fluoxetine. Its half-life is over two weeks. You’d need to stop for weeks to see a difference, and that’s not safe. There’s a catch: stopping suddenly can cause withdrawal symptoms like dizziness, nausea, or anxiety. About 15% to 20% of people experience this. If you’ve been on the medication for more than a few months, even a short break can trigger discomfort. So, this approach only makes sense if you’re on a short-acting SSRI, have a stable mood, and are planning ahead for intimacy.Switching Antidepressants
If dose changes and drug holidays don’t help, switching to a different antidepressant is the next step. Not all SSRIs are equal when it comes to sexual side effects. Paroxetine is the worst offender. Sertraline and fluoxetine are better, but still cause problems for many. Bupropion (Wellbutrin) is often the go-to switch because it doesn’t raise serotonin-it boosts dopamine and norepinephrine instead. That’s why it doesn’t hurt sexual function. In fact, 60% to 70% of people who switch from an SSRI to bupropion see major improvement. But switching isn’t simple. Bupropion takes 2 to 4 weeks to reach full effect. And if you have severe depression, switching increases your risk of relapse to 25% to 30%. That’s higher than staying on your SSRI, where relapse risk is only 10% to 15%. Mirtazapine and nefazodone are other options-they block certain serotonin receptors and can improve sexual function in about half of users. But they make you sleepy, and that’s not ideal for everyone.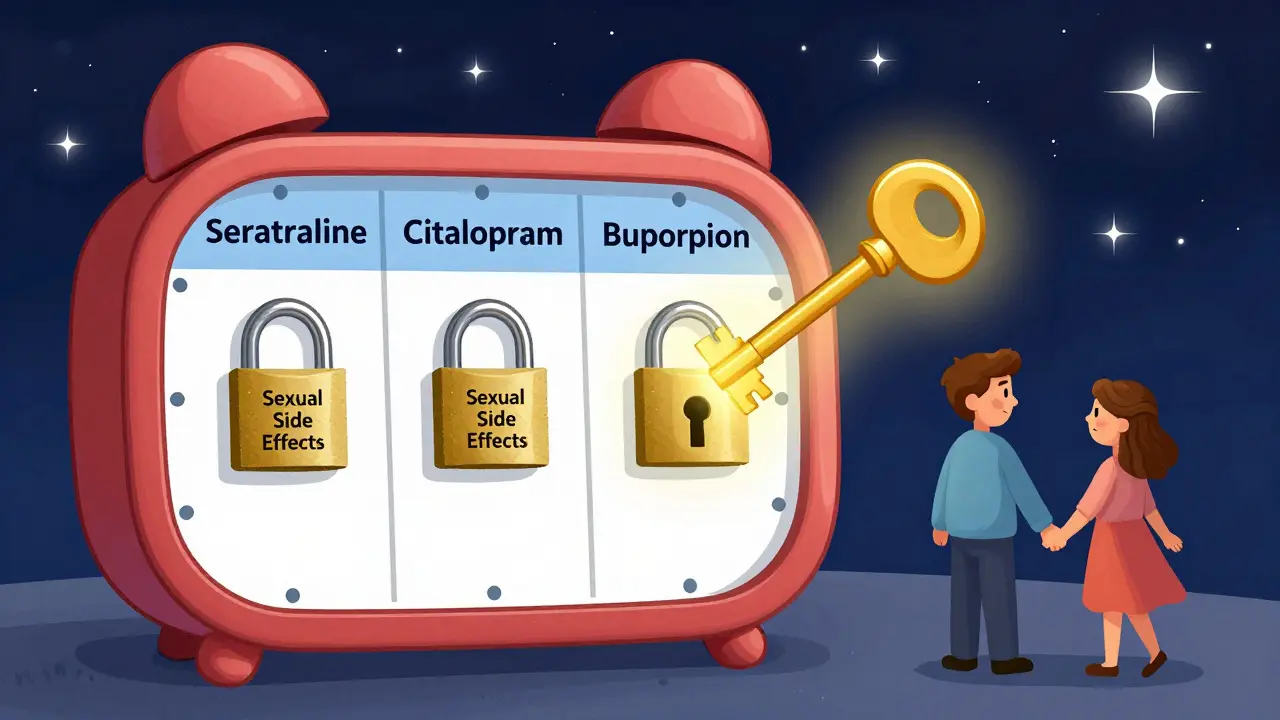
Adding Bupropion as an Adjunct
Instead of switching, you can add bupropion to your current SSRI. This is the most studied and effective approach. In a double-blind trial of 55 people on citalopram, fluoxetine, paroxetine, or sertraline, adding bupropion led to 66% improvement in sexual desire and frequency when taken daily at 150mg twice a day. That’s better than switching. For those who don’t want to take it every day, an as-needed dose of 75mg of immediate-release bupropion taken 1 to 2 hours before sex helped 38% of users. That’s good-but not as good as daily use. The downside? About 20% to 25% of people report increased anxiety, especially if they’re already on fluoxetine. So, if you’re prone to panic attacks or jitteriness, this might not be for you.Other Adjuncts: Dopaminergic and Serotonergic Options
If bupropion doesn’t work or causes too much anxiety, there are other options. Dopaminergic drugs like ropinirole (used for Parkinson’s) and amantadine can help. They kick in fast-within 48 to 72 hours-and improve sexual function in 40% to 50% of users. But they can cause tremors, dizziness, or anxiety, especially when mixed with SSRIs. Discontinuation rates are higher here too, around 30%. Buspirone (Buspar), a 5-HT1A partial agonist, is another choice. Taken daily at 5 to 15mg, it improves sexual function in 45% to 55% of people. It’s safer than dopamine drugs, with only 5% to 10% stopping due to side effects. The catch? It takes 2 to 3 weeks to work. If you need quick results, this isn’t it. Cyproheptadine is an older antihistamine that blocks serotonin receptors. At 2 to 4mg as needed, it helps about half of users. But it causes drowsiness in 35% to 40% of people. It’s not a first-line option, but for some, it’s the only thing that works.Behavioral Strategies: More Than Just Pills
Medication isn’t the whole story. Some of the most effective fixes are non-pharmacological. Dr. Levine, a leading psychiatrist, says most patients under 60 don’t have complete anorgasmia-they just feel like the pleasure is muted. He suggests trying new sexual activities, more stimulation, or even changing the timing or setting. One patient on Reddit said switching from intercourse to oral sex and adding vibrators helped her finally reach orgasm again. Couples who practiced “sensate focus”-a therapy technique where partners take turns touching without pressure to have sex-reported 50% improvement in satisfaction, even while still on SSRIs. It’s about reconnecting with pleasure, not just performance. And that’s powerful.Persistent Sexual Dysfunction: The Lingering Risk
There’s a scary possibility: sexual side effects that stick around after you stop the SSRI. The Therapeutic Goods Administration (TGA) issued a warning in June 2023 about this. Some people report problems lasting months-or even years-after quitting. A 2022 survey from SSRI Stories found that 37% of respondents had ongoing issues six months or longer after stopping. That’s rare, but it’s real. Some experts argue we don’t yet have solid proof that SSRIs cause this. A 2023 systematic review found only 8 studies out of hundreds met rigorous standards. But the fact that it’s been reported by thousands of people means we can’t ignore it. If you’re thinking about stopping your SSRI, talk to your doctor about this risk. Don’t assume it’ll just go away.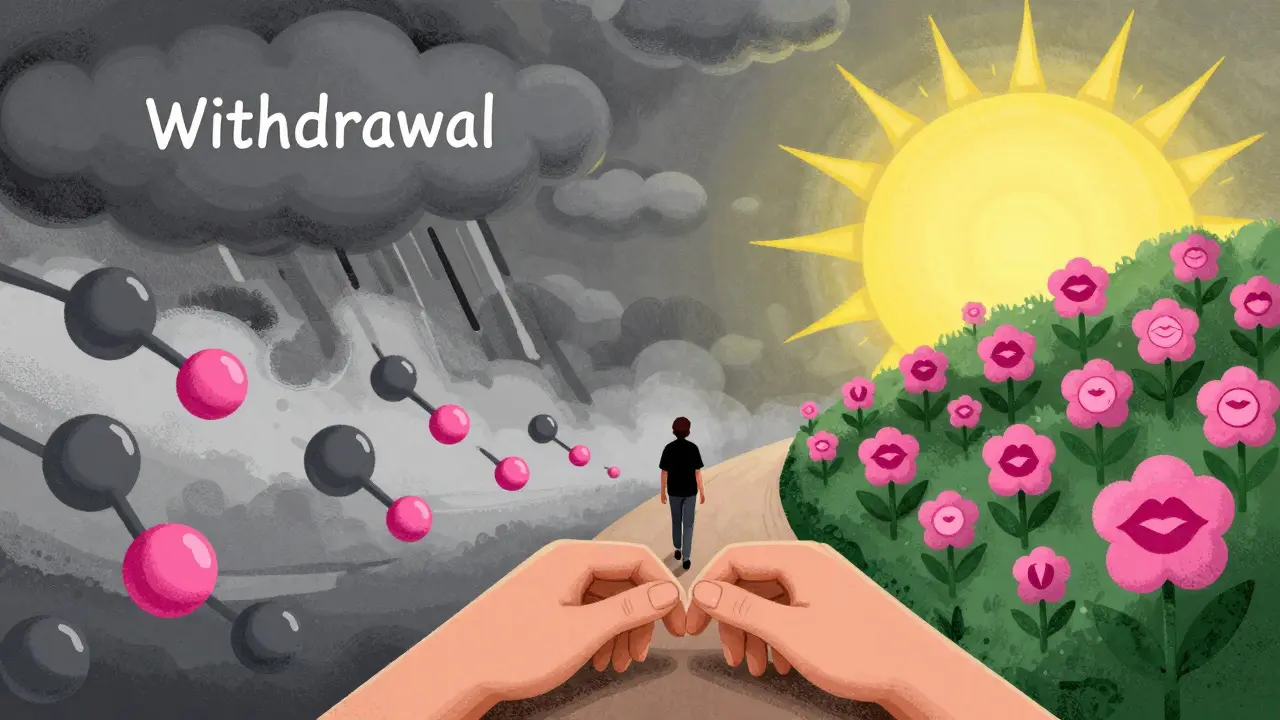
What Works Best? A Quick Guide
- Best for quick results: As-needed bupropion (75mg) or dopaminergic agents like ropinirole
- Best for long-term improvement: Daily bupropion (150mg twice daily)
- Best safety profile: Buspirone
- Best for short-acting SSRIs: Drug holidays (48-72 hours)
- Best overall success rate: Adding bupropion to your current SSRI
- Best for people who can’t take stimulants: Switching to mirtazapine or nefazodone


Comments (8)
Alvin Bregman
January 13, 2026 AT 16:35ive been on sertraline for 3 years and my sex life is basically a ghost story now
tried lowering the dose to 50mg and it barely made a difference
then i tried skipping it for 2 days before sex and it worked like magic
until i got the shakes and felt like i was dying for 12 hours
so now i just accept it
its not the meds its the world
Sarah -Jane Vincent
January 15, 2026 AT 09:20you think this is bad wait until you find out the FDA knew about this for 20 years and buried the studies
pharma companies paid off the psychiatrists who told you this was normal
they even funded the research that says bupropion helps
its all a scam to keep you dependent
why do you think they push the 150mg twice daily dose
because they make more money off the brand name
and dont get me started on the long term dysfunction
thats not a side effect thats a coverup
theyre testing this on you like guinea pigs
and now you think its your fault for not trying hard enough
wake up
Henry Sy
January 15, 2026 AT 16:18yo i tried the bupropion add-on and it was like my brain turned into a jackhammer
one day i was chill on my ssri then boom
next day i was sweating bullets and yelling at my cat for breathing too loud
then i tried the 75mg as needed
got a boner but felt like i was gonna pass out
so i went full analog
no meds no drama
just me my partner and a damn vibrator
and guess what
i came
for the first time in 4 years
not because of science
because i stopped letting doctors decide what pleasure looks like
Anna Hunger
January 16, 2026 AT 22:27It is imperative to emphasize that any modification to pharmacological regimens must be undertaken exclusively under the supervision of a licensed clinical practitioner.
The literature consistently demonstrates that abrupt discontinuation or unsupervised dose adjustment of SSRIs carries a significant risk of discontinuation syndrome, which may manifest as neurological, gastrointestinal, or affective disturbances.
Furthermore, the adjunctive use of bupropion, while statistically supported in controlled trials, may precipitate hypertensive crises or seizures in patients with preexisting risk factors.
It is also noteworthy that behavioral interventions such as sensate focus are empirically validated and should be considered first-line adjuncts prior to polypharmacy.
Patients are encouraged to maintain detailed symptom logs and to engage in shared decision-making with their providers.
Self-experimentation, while often emotionally compelling, is neither safe nor clinically advisable.
Andrew Freeman
January 17, 2026 AT 21:00drug holidays work if you dont have a brain
my doc said no because i might relapse
so i relapsed anyway
but at least i got to cum
worth it
says haze
January 18, 2026 AT 14:42the real tragedy here is not the sexual dysfunction
it’s the way we’ve reduced intimacy to a pharmacological problem
we’ve turned touch into a dosage calculation
orgasm into a side effect metric
and love into a risk-benefit analysis
we’re not treating depression anymore
we’re optimizing libido
and in doing so
we’ve lost the poetry of desire
the messy
unquantifiable
human thing
that existed before the pill
Jason Yan
January 19, 2026 AT 10:21look i get it
we all want to fix this fast
we want the pill the trick the hack
but here’s what no one tells you
the body remembers
when you stop chasing orgasm like it’s a finish line
when you start touching just to feel
when you let silence sit between you and your partner
that’s when the pleasure comes back
not because of bupropion
not because of a drug holiday
but because you stopped treating your sexuality like a broken machine
and started treating it like a relationship
and relationships take time
and patience
and a lot of bad jokes in the dark
and that’s okay
shiv singh
January 20, 2026 AT 15:37you people are so selfish
you care more about your dick than your mental health
if you were really depressed you’d be grateful for any relief
you think you’re entitled to sex
like its a right
while you sit there complaining about your meds
while people in war zones die without antidepressants
get over yourself
your libido is not a human right
your depression is