Uric Acid & Kidney Stones Risk Calculator
Enter your information and click "Calculate Your Risk" to see your personalized risk assessment.
Types of Kidney Stones
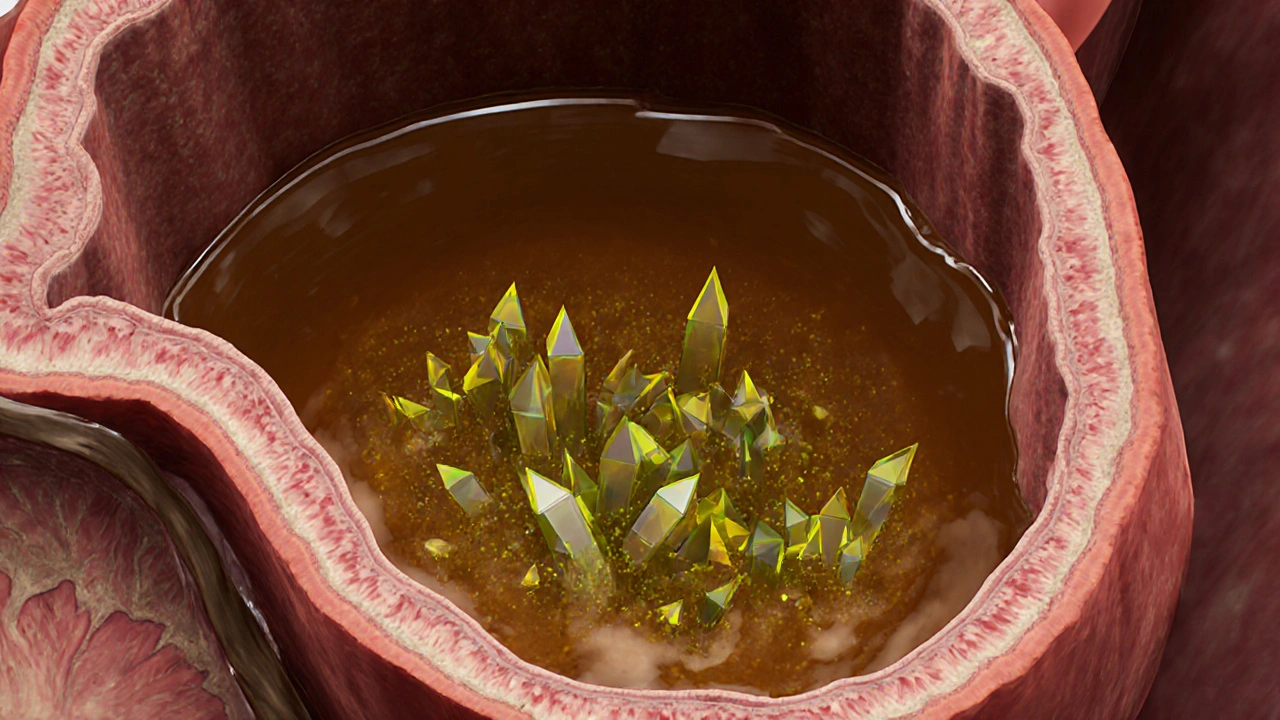
Uric Acid Stones
Directly linked to high uric acid levels. Often smooth and may pass more easily.
Calcium Oxalate Stones
Most common type. Form when calcium combines with oxalate in urine.
Ever wondered why some people repeatedly develop painful kidney stones while others never do? One often‑overlooked factor is the level of high uric acid in the blood. Understanding how this chemical builds up, how it interacts with kidney function, and what you can do to keep it in check can dramatically cut your risk of stone formation.
What Is Uric Acid and What Counts as High?
Uric acid is a waste product created when the body breaks down purines - substances found in many foods and also produced by cells. Uric Acid is a crystalline compound that normally dissolves in the bloodstream and is expelled via the kidneys in urine. Normal serum levels range from about 3.5 to 7.0 mg/dL for men and 2.5 to 6.0 mg/dL for women. Anything consistently above these thresholds is called Hyperuricemia an elevated blood uric acid condition that can trigger gout attacks and crystal deposits in tissues. Genetics, diet, obesity, and certain medications can push levels into the risky zone.
Kidney Stones 101: Types and How They Form
Kidney stones are solid masses that develop from minerals and salts that precipitate in the urinary tract. The most common types are:
- Calcium oxalate stones - account for about 70% of cases.
- Uric acid stones - make up roughly 10% and are directly linked to high uric acid.
- Struvite stones - often result from chronic urinary infections.
- Cystine stones - rare, caused by a genetic disorder.
All stones share a common pathway: supersaturation of urine with a particular compound, tiny crystals forming, then aggregating into a stone that can lodge in the kidney, ureter, or bladder.
How High Uric Acid Turns Into Stones
When uric acid levels climb, two things happen that set the stage for stone formation:
- Acidic urine - Uric acid is more likely to stay in solid form when the urine pH drops below 5.5. Acidic urine reduces the solubility of uric acid, letting crystals appear.
- Crystal nucleation - Excess uric acid provides a seed around which other minerals, especially calcium, can attach. This mixed crystal can grow into a larger stone.
People with hyperuricemia often experience repeated “gout‑like” attacks in the joints, but the same crystals can lodge in the renal tubules, creating what doctors call uric acid kidney stones. These stones are usually smoother and can pass more easily than calcium oxalate stones, yet they still cause severe flank pain, blood in urine, and nausea.
Risk Factors That Compound the Problem
High uric acid rarely acts alone. Several lifestyle and medical conditions amplify the danger:
- Obesity - increases production of purines and reduces urine pH.
- Dehydration - concentrates urine, making it easier for crystals to reach supersaturation.
- Diabetes - can cause acidic urine and higher uric acid output.
- Excessive intake of Purine‑rich foods - organ meats, anchovies, sardines, and certain legumes.
- Long‑term use of Diuretics - promote fluid loss and raise uric acid concentration.
Identifying which of these apply to you helps tailor prevention strategies.
Testing and Diagnosis
If you suspect a uric acid issue, two simple labs give the picture:
- Serum uric acid test - measures the concentration in blood. Values above 7.0 mg/dL for men and 6.0 mg/dL for women typically flag hyperuricemia.
- Urine pH test - a dipstick or 24‑hour collection tells you how acidic your pee is. A pH under 5.5 hints that uric acid stones could form.
Imaging, such as a non‑contrast CT scan, confirms stone size and location. If the stone composition can be analyzed (often after it passes), labs can confirm it is mainly uric acid.
Diet and Lifestyle Tweaks to Lower Uric Acid
Changing what you eat and how you hydrate can bring uric acid back into a safe zone. Here’s a practical checklist:
- Drink at least 2‑3 liters of water daily; aim for clear, pale urine.
- Limit red meat and organ meats to once a week or less.
- Swap high‑purine fish (sardines, anchovies) for low‑purine options like salmon or white fish.
- Replace sugary sodas with water or herbal tea; fructose spikes uric acid production.
- Eat more low‑purine vegetables (bell peppers, carrots, cabbage) and fruits (cherries are especially helpful).
- Include alkaline‑forming foods - dairy, nuts, and most fruits - to raise urine pH.
- Maintain a healthy weight; losing 5‑10% of body weight can lower uric acid by up to 20%.
For those who struggle to keep urine pH high, doctors may prescribe potassium citrate or sodium bicarbonate to buffer acidity.
Medications That Target Uric Acid
When lifestyle changes aren’t enough, medication steps in:
- Allopurinol - reduces uric acid production by inhibiting the enzyme xanthine oxidase.
- Febuxostat - a newer xanthine oxidase inhibitor used when allopurinol isn’t tolerated.
- Probenecid - increases kidney excretion of uric acid.
These drugs are most effective when paired with adequate hydration and a low‑purine diet. Always discuss potential side effects and dosing with a physician.

Comparison of Kidney Stone Types
| Type | Primary composition | Typical pH range | Common risk factors | Prevention focus |
|---|---|---|---|---|
| Calcium oxalate | Calcium + oxalate | 6.0‑7.0 (neutral) | High oxalate foods, low calcium intake, hypercalciuria | Increase dietary calcium, limit oxalates, stay hydrated |
| Uric acid | Uric acid crystals | <5.5 (acidic) | Hyperuricemia, gout, high‑purine diet, dehydration | Alkalinize urine, lower purine intake, boost water |
| Struvite | Magnesium ammonium phosphate | 7.0‑8.0 (alkaline) | Recurrent UTIs, kidney infections | Treat infections promptly, maintain urine flow |
| Cystine | Cystine | 5.0‑7.0 (varies) | Genetic cystinuria, high cystine excretion | Large fluid intake, alkalinizing agents |
When to Seek Professional Help
If you experience any of the following, schedule a medical appointment promptly:
- Severe, sudden flank pain radiating to the groin.
- Blood in urine or persistent cloudy urine.
- Nausea, vomiting, or fever accompanying pain.
- Repeated stone episodes despite diet changes.
Early intervention can prevent larger stones that require surgical removal. Your doctor may recommend shock‑wave lithotripsy, ureteroscopy, or percutaneous nephrolithotomy depending on stone size and location.
Quick Takeaways
- High uric acid makes urine acidic, encouraging crystal formation.
- Stay well‑hydrated and keep urine pH above 5.5 to dissolve uric acid.
- Cut purine‑rich foods, manage weight, and consider alkalinizing agents.
- Blood test and urine pH check are simple ways to monitor risk.
- Medication like allopurinol works best alongside lifestyle shifts.
Frequently Asked Questions
Can a uric acid stone dissolve on its own?
If urine stays alkaline (pH>6.5) and you drink plenty of fluids, many small uric acid stones can dissolve without intervention. However, larger stones often need medical treatment.
Is there a direct link between gout and kidney stones?
Yes. Both conditions stem from excess uric acid. People with frequent gout attacks have a higher likelihood of developing uric acid stones.
How many glasses of water should I drink to prevent stones?
Aim for at least 2‑3liters a day (about 8‑12 glasses). The goal is to produce at least 2liters of urine each day.
Are there any foods that actively raise urine pH?
Dairy products, almonds, and most fruits are alkaline‑forming and help raise urine pH. Adding a small glass of lemon water daily can also have a mild alkalizing effect.
What role does potassium citrate play in stone prevention?
Potassium citrate supplies citrate, which binds calcium and makes urine less acidic. It’s commonly prescribed for patients with recurrent uric acid or calcium oxalate stones.

Comments (17)
Shana Shapiro '19
October 11, 2025 AT 12:11I understand how unsettling it can be to discover elevated uric acid levels. The idea that this could lead to painful kidney stones adds genuine worry. You are not alone-many people experience the same concerns and have found relief through simple adjustments. Increasing water intake, moderating purine‑rich foods, and staying active often makes a noticeable difference. Keep monitoring your labs and stay in touch with your healthcare provider.
Jillian Bell
October 15, 2025 AT 10:38Don't be fooled by the glossy pamphlets the pharma industry pushes. They want you to think you only need a couple of pills, while the real solution lies in exposing the hidden agenda behind water fluoridation and food additives that raise uric acid silently. Wake up, question the data, and demand natural alternatives.
Lindsey Bollig
October 19, 2025 AT 09:05Great rundown! If you’re looking to lower uric acid, try swapping out organ meats for lean chicken and add more cherries to your diet – they’ve been shown to help. Also, sipping lemon‑water throughout the day can give a gentle alkalizing boost. Keep up the hydration and you’ll likely see your numbers drop over a few weeks.
Daniel Buchanan
October 23, 2025 AT 07:31One practical tip: set a reminder on your phone to drink a glass of water every hour. It’s a small habit that builds up to the 2‑3 liters most guidelines suggest. Pair that with a short walk after meals to help your metabolism process purines more efficiently.
Lena Williams
October 27, 2025 AT 04:58Yo, I was scrolling through the article and thought, "okay, that's a lot of info, but lemme break it down for the crew." First off, uric acid is basically a waste product from breaking down purines, which are in a ton of foods like beef, sardines, and even some veges. If you eat a lot of that stuff, your blood can get loaded and the kidneys have to work overtime to dump it. When the pee gets acidic – less than about 5.5 pH – the uric acid decides to crystal‑ize, kinda like sugar when you bake a cake and it forms candy shards. Those tiny crystals can stick together and become a stone, which is super painful when they try to move. Some folks think it’s just a gout thing, but actually the same crystals can lodge right in the renal tubules. The article mentions staying hydrated – that’s the #1 move, because dilution keeps your urine from getting supersaturated. Also, dropping the heavy‑purine foods helps lower the overall production, and swapping to chicken or tofu can make a big dent. A word about soda – the high fructose corn syrup in many soft drinks is a sneaky catalyst for uric acid spikes, so ditching those is wise. I’ve also read that a handful of cherries a day can actually lower uric acid levels, so that’s a tasty hack. If you’re on diuretics, you might need to be extra careful because they concentrate your urine and raise uric acid further. Bottom line: watch your diet, drink water like it’s your job, and consider talking to a doc about possible meds if lifestyle tweaks don’t cut it.
Sierra Bagstad
October 31, 2025 AT 03:25According to current nephrology guidelines, serum uric acid exceeding 7.0 mg/dL in men and 6.0 mg/dL in women constitutes hyperuricemia, which correlates with an increased incidence of uric acid nephrolithiasis. The solubility product of uric acid decreases markedly at urine pH values below 5.5, facilitating crystal nucleation. Dietary purine restriction, adequate hydration, and, when indicated, xanthine oxidase inhibition constitute the cornerstone of management.
Alan Kogosowski
November 4, 2025 AT 01:51From a pathophysiological perspective, the interplay between renal tubular handling of uric acid and systemic metabolic factors is elegantly complex. For instance, insulin resistance can impair uric acid excretion, thereby creating a feedback loop that predisposes to stone formation. Moreover, the role of gut microbiota in purine metabolism is an emerging field that may soon reshape our therapeutic approaches. While the article provides a solid clinical overview, future research might benefit from integrating these molecular insights.
Ben Lee
November 8, 2025 AT 00:18I appreciate the thoroughness of the guide. Adding a quick tip: a squeeze bottle of lemon juice in your water can subtly raise urine pH, which helps keep uric acid dissolved. Also, if you’re already drinking the recommended volume, consider timing your water intake around meals to maximize dilution when purine load peaks.
David Brice
November 11, 2025 AT 22:45Listen up – you cant just rely on "drink more water" if you keep chugging soda and pizza. Cut the junk, get real, and talk to your doc about allopurinol if diets dont cut it. I dug into the data and it says the same. And yeah, stay consistent, no excuses.
Zachary Schroer
November 15, 2025 AT 21:11Really? Another "eat more water" post… 🙄🥤💧
Stacy Whitman
November 19, 2025 AT 19:38Only americans think kidney stones are a big deal.
Kim and Lin
November 23, 2025 AT 18:05Nice info! 😀 I’ll start adding a glass of lemon water each morning and swap out the steak for chicken. Also, will keep an eye on my urine pH with those test strips.
Kemari Nielson
November 27, 2025 AT 16:31Solid article, concise and practical.
Steve Helsel
December 1, 2025 AT 14:58Meh, same old advice – drink water, cut meat. Nothing revolutionary here.
Steve Moody
December 5, 2025 AT 13:25While the piece admirably covers the basics – hydration, dietary purine moderation, urine pH considerations – it conspicuously glosses over the nuanced pharmacologic landscape; for instance, the differential tolerability profiles of allopurinol versus febuxostat merit explicit mention, as does the potential utility of uricosuric agents such as probenecid in select patients; likewise, the emerging role of potassium citrate not merely as a pH buffer but as a crystallization inhibitor is an omission that warrants correction; finally, the interplay between metabolic syndrome components and uric acid handling could be explored with greater depth, thereby enriching the clinician’s toolkit beyond the surface‑level recommendations currently presented.
Adrian Hernandez
December 9, 2025 AT 11:51Everyone forgets that the water they drink is often filled with micro‑plastics that can affect kidney function.
duncan hines
December 13, 2025 AT 10:18Whoa, hold up – that "quick tip" about lemon water? You’re basically telling folks to pour acid into already acidic urine. That’s a recipe for more stones, not fewer! Honestly, the article should have warned about the potential pH swing. People need real science, not just feel‑good hacks. And by the way, the typo “uric acid” as “uric aci” in the table? Sloppy editing at best.