What if your pain isn’t telling you your body is broken?
Most people think pain means damage. If your back hurts, you assume a disc is out of place. If your knee aches, you think the cartilage is worn out. That’s what doctors used to tell us. But science now shows something very different: pain is not a direct message from injured tissue. It’s a warning signal your brain creates - sometimes way too loudly.
This is the core idea behind Pain Neuroscience Education, or PNE. It’s not a treatment like massage or exercise. It’s a way of teaching your brain that pain doesn’t always mean danger. And when you change how you think about pain, your body often responds by hurting less - even if nothing physically changes.
Why traditional pain advice often makes things worse
For decades, pain was treated like a broken pipe. If you had back pain, you were told to rest, avoid bending, and fear movement. You got X-rays showing "degenerative changes" - worn discs, bone spurs, arthritis - and were told these were the cause. That made sense. But here’s the problem: many people with "severe" spinal changes on scans feel no pain at all. And many with intense, daily pain have perfectly normal scans.
When you’re told your body is damaged and you must protect it, your brain goes into survival mode. You stop moving. You avoid activities. You start worrying every twinge is a sign of ruin. This fear becomes a loop: less movement → more sensitivity → more fear → more pain. It’s not your tissues getting worse. It’s your nervous system becoming hypersensitive.
That’s why rest and avoidance often backfire. A 2023 review of 23 studies found patients who were told to "protect their spine" showed no improvement in pain or function - while those who learned how pain really works improved significantly.
How PNE works: The brain’s alarm system
PNE teaches you that pain is like a smoke alarm. It’s not designed to tell you if there’s fire. It’s designed to tell you there’s possible danger - and it’s often overly sensitive.
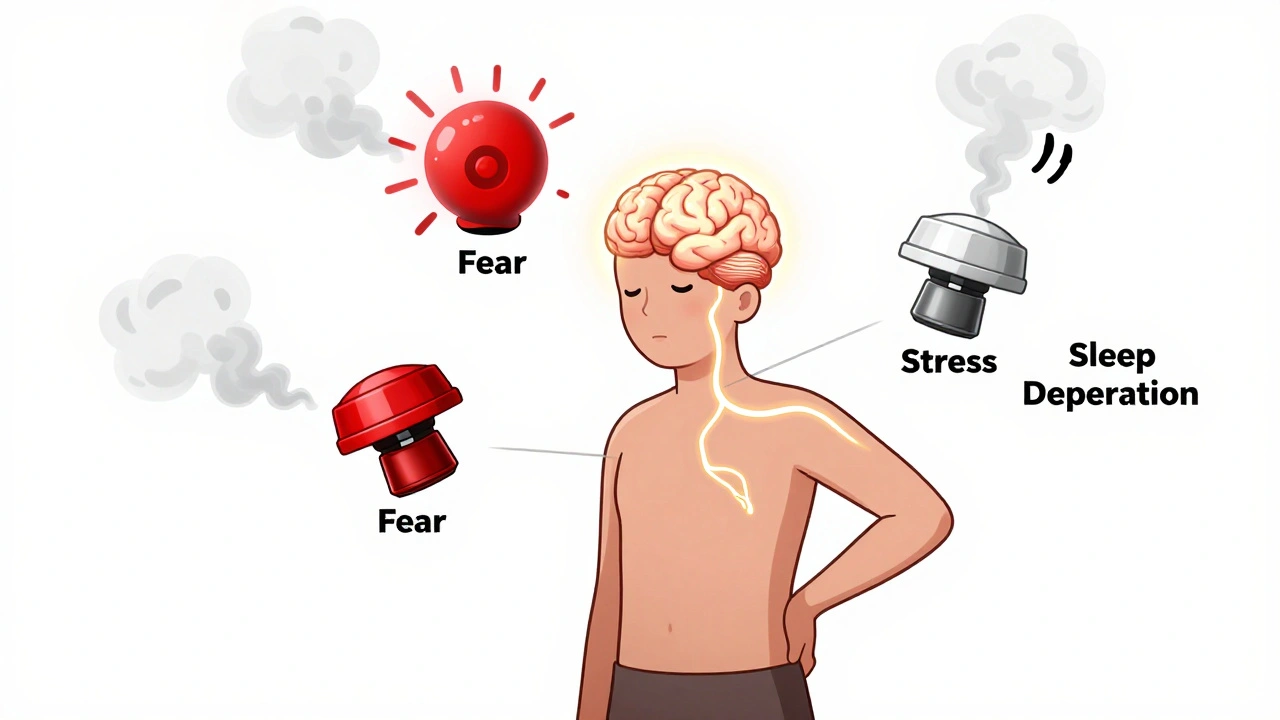
When you have chronic pain, your nervous system gets stuck in high alert. Your nerves become more responsive. Your spinal cord amplifies signals. Your brain starts interpreting even normal movements as threats. This is called central sensitization. It’s not imaginary. It’s real neurobiology.
PNE explains this using simple metaphors, diagrams, and stories. Instead of saying "your disc is bulging," you learn: "Your nerves are on edge. Your brain is overprotective. Your pain system is stuck in a loop."
One common metaphor is the "volume knob." Your pain isn’t a switch - it’s a dial. Stress, sleep, emotions, movement, and even your beliefs can turn it up or down. You’re not powerless. You can turn it down - not by avoiding pain, but by understanding it.
What happens when you learn this?
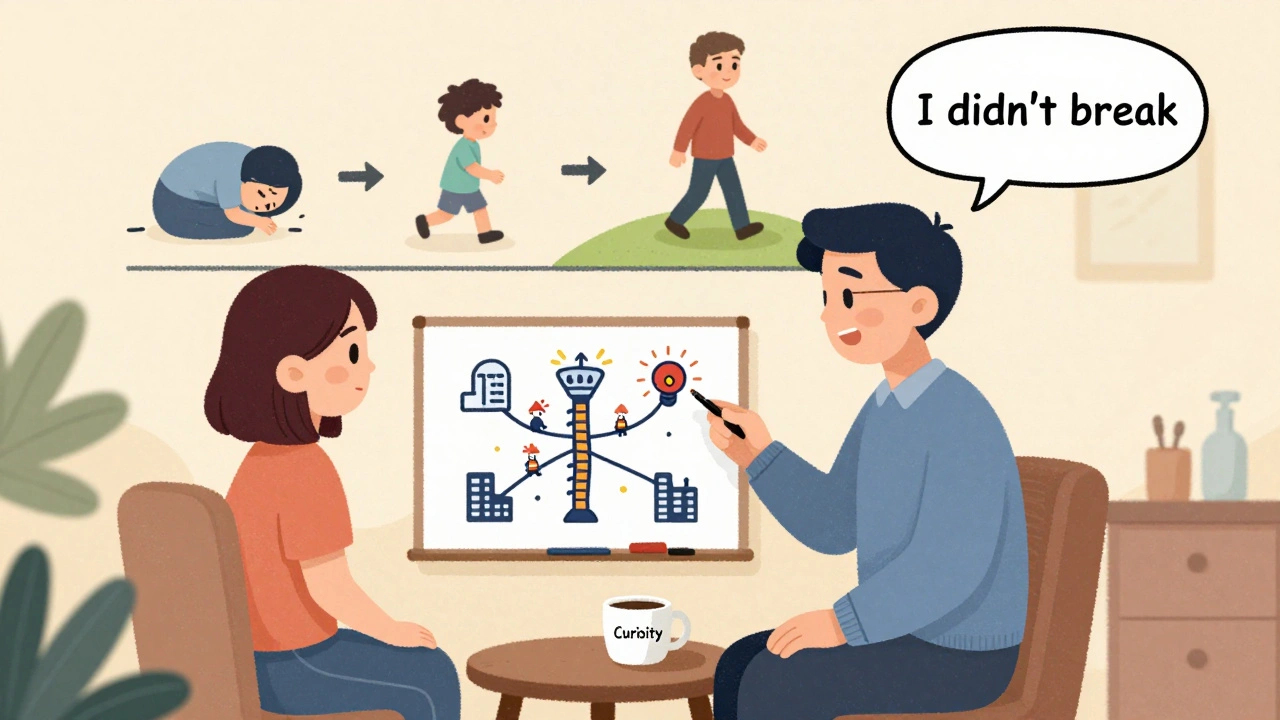
When patients truly understand PNE, something shifts. They stop seeing pain as a signal to freeze. They start seeing it as a signal to move - slowly, safely, and with curiosity.
Studies show PNE leads to measurable changes:
- Pain intensity drops by an average of 1.8 points on a 10-point scale - enough to notice in daily life.
- Disability improves by over 12% - meaning people can walk farther, lift more, sleep better.
- Pain catastrophizing (the habit of imagining the worst) drops by more than 6 points on a standard scale.
And it’s not just numbers. Real people report real changes. One patient in Birmingham, a 42-year-old nurse with fibromyalgia, cut her daily pain medication from six pills to one every three days after six PNE sessions combined with gentle movement. She didn’t get "cured." But she got her life back.
Another Reddit user, who’d been afraid to hike for years, described the moment it clicked: "I realized my pain wasn’t a fire alarm - it was a smoke alarm. It was just being too sensitive. So I walked up the hill. And I didn’t break."

PNE isn’t magic. It’s not a quick fix.
Some people expect PNE to erase pain overnight. It doesn’t. It doesn’t fix structural issues. It doesn’t replace exercise. It doesn’t make your disc regenerate.
What it does is remove the fear that keeps pain stuck. When you stop fearing movement, your body relaxes. When you stop believing pain equals damage, your nervous system calms down. Then - and only then - can movement, exercise, and therapy work better.
Research shows PNE alone helps. But when you add it to movement therapy, the results jump. One study found patients who got PNE + exercise improved 30-40% more than those who got exercise alone. That’s not small. That’s life-changing.
Who benefits most from PNE?
PNE works best for people with chronic pain - pain lasting more than three months - where scans don’t match symptoms. This includes:
- Chronic low back pain
- Fibromyalgia
- Chronic neck pain
- Tennis elbow that won’t heal
- Persistent knee pain without clear injury
It’s less helpful for acute injuries - like a broken bone or recent surgery - where tissue damage is clearly the issue. In those cases, rest and healing come first.
It also doesn’t work well for people with severe cognitive challenges or very low health literacy. If someone can’t follow a story about nerves and alarms, the science becomes confusing - not helpful.
How is PNE delivered?
PNE is usually given by a physical therapist, occupational therapist, or pain specialist trained in neuroscience education. Sessions are typically 30-45 minutes, often done in person, one-on-one.
Good PNE doesn’t feel like a lecture. It feels like a conversation. Therapists use:
- Simple drawings of nerves and the brain
- Metaphors like smoke alarms, volume knobs, and alarm systems
- Real-life examples: "Think about how you feel when you’re exhausted or stressed - even a light touch can hurt more. That’s your nervous system being sensitive."
- Written handouts and digital tools (apps like Pain Revolution help reinforce learning)
Many clinics now include PNE as part of standard care. In the U.S., 68% of pain-specialized physical therapy clinics offer it. In the UK, it’s growing fast - especially in NHS pain clinics.
What if you’re skeptical?
It’s normal to doubt this. After all, your pain feels real. And if your doctor told you your spine was damaged, why would you believe it’s just your brain being loud?
Here’s the key: you don’t have to believe it right away. You just have to be curious. Ask yourself: "Could my pain be more about my nervous system than my spine?" Even if you’re not sure, try the movement. Try the breathing. Try the gentle walk. See what happens.
One of the most powerful parts of PNE is that it doesn’t ask you to deny your pain. It asks you to understand it. And understanding gives you back control.
Getting started: What you can do today
You don’t need to wait for a therapist to begin learning about pain neuroscience.
Start here:
- Read the first chapter of Explain Pain by David Butler and Lorimer Moseley. It’s written for patients, not doctors.
- Watch the 10-minute video "The Painful Brain" by Lorimer Moseley on YouTube. It’s clear, simple, and powerful.
- Next time you feel pain, pause. Ask: "Is this a signal to stop - or a signal to move slowly?" Don’t judge. Just notice.
- Try one small movement you’ve been avoiding. A short walk. A gentle stretch. See what happens. Don’t push through pain. But don’t run from it either.
Change doesn’t happen in one day. But it starts with one new thought: Pain is not a measure of damage. It’s a measure of threat.
What’s next for pain education?
PNE is evolving. Researchers are testing virtual reality versions that immerse patients in 3D animations of their own nervous system. Others are using brain scans to personalize the message - showing exactly how stress or sleep affects pain pathways in real time.
Insurance companies are catching on too. In the U.S., Medicare now pays for PNE as part of physical therapy. Employers are using it to cut workers’ comp claims. Hospitals are integrating it into post-surgery rehab.
The message is clear: pain is not just a physical problem. It’s a brain problem. And the brain can be retrained.
Final thought: You’re not broken. Your alarm system is just too loud.
Chronic pain doesn’t mean you’re weak. It doesn’t mean you’re failing. It means your nervous system has learned to sound the alarm too easily.
PNE doesn’t promise to make your pain vanish. But it gives you the tools to stop letting it control you. You can move. You can live. You can heal - not because your body changed, but because your mind did.
That’s not magic. That’s science. And it’s working - for thousands of people, right now, in clinics and homes across the UK and beyond.
Is pain neuroscience education only for back pain?
No. PNE works for any chronic pain condition where the nervous system has become overly sensitive - including fibromyalgia, chronic neck pain, persistent headaches, knee pain without injury, and even long-term shoulder pain. It’s most effective when pain lasts longer than three months and doesn’t match up with imaging results.
Can I do PNE on my own, or do I need a therapist?
You can start learning on your own with books or videos - but working with a trained therapist gives you personalized feedback and helps you connect the science to your daily movements. A therapist can spot when you’re still avoiding activities due to fear, even if you think you understand the concepts. The best results come from combining self-learning with guided sessions.
Does PNE mean my pain isn’t real?
Absolutely not. Your pain is real - but it’s not always caused by tissue damage. Think of it like a fever: it’s real, but it’s not the illness itself. It’s your body’s response. PNE helps you understand that your pain is your nervous system’s response - often too strong - and that you can help calm it down.
How long does it take to see results from PNE?
Many people notice a shift in how they think about pain after just one or two sessions. But real changes in movement, confidence, and pain levels usually take 4-6 weeks of applying the ideas - especially when combined with gentle movement. It’s not about fixing your body. It’s about changing your relationship with pain.
Is PNE covered by insurance?
In the U.S., Medicare and many private insurers cover PNE when delivered by a licensed physical therapist under standard evaluation codes (CPT 97160-97164). In the UK, it’s increasingly offered in NHS pain clinics, though availability varies by region. Always ask your provider if they offer neuroscience-based pain education as part of treatment.
What if PNE doesn’t work for me?
If you don’t feel it’s helping, it might be because you’re still expecting pain to disappear - not change. PNE works best when you’re open to learning, not fixing. Some people need more time. Others benefit from combining it with other therapies like graded exposure or mindfulness. If you’re still stuck, talk to your therapist about adjusting the approach - or exploring other tools like cognitive behavioral therapy.

Comments (15)
Ali Bradshaw
December 4, 2025 AT 23:16This is the kind of post that makes me want to hug my physical therapist. I had back pain for years, thought I was broken. Turns out my brain was just screaming at me for skipping sleep and stressing over work. Started moving again - slowly - and now I hike on weekends. No magic. Just science.
Thank you for writing this.
Rupa DasGupta
December 5, 2025 AT 02:59I get it but also... what if your brain is just broken? Like, what if it's not overreacting - what if it's *correctly* sensing something no scan can catch? 🤔 I’ve had pain for 7 years. No one believes me. So now I just believe me.
Deborah Jacobs
December 5, 2025 AT 09:21I used to think pain was a moral failure - like if I just tried harder, I wouldn’t hurt. Then I learned pain isn’t a punishment. It’s a miscommunication. My therapist drew a smoke alarm on a napkin and I cried. Not because I was sad - because for the first time, I didn’t feel guilty for hurting.
Thank you for saying this out loud.
ashlie perry
December 6, 2025 AT 13:18Pain is real but its not damage its just your brain being dramatic like a teenager with a broken phone
Lucy Kavanagh
December 7, 2025 AT 00:18This is why the NHS is falling apart. You don’t fix chronic pain by talking about smoke alarms. You fix it with real medicine. Strong painkillers. Injections. Surgery. Not some New Age brain whispering. We’ve got real problems here - not metaphors.
Marvin Gordon
December 7, 2025 AT 18:33I used to be Lucy’s type - skeptical, angry, thought I was broken. Then I read Explain Pain. Didn’t change my MRI. But it changed how I moved. I started walking 10 minutes a day. Then 20. Then I rode a bike again. No surgery. No miracle. Just stopped listening to fear. Your brain listens when you stop screaming at it.
Harry Nguyen
December 8, 2025 AT 11:28So let me get this straight - if I have a herniated disc and it’s pressing on a nerve, but my pain is "just a smoke alarm"... then why does my leg go numb when I sit? Is my leg also being dramatic? This is just science-speak for "your pain is in your head" which is what doctors told me in 1998 and I still can’t walk without a cane.
Philip Kristy Wijaya
December 10, 2025 AT 09:29The notion that pain is merely a neurobiological construct is a convenient fiction peddled by pharmaceutical-adjacent institutions to absolve themselves of responsibility for structural degeneration. One cannot dismiss the physical reality of osteophytic hypertrophy or annular fissures as mere "overactive alarms" - this is cognitive dissonance masquerading as enlightenment. The reductionist paradigm of neuroscience education serves to depoliticize suffering and redirect blame onto the victim’s neurochemistry - a profoundly dangerous epistemological shift.
Jimmy Jude
December 11, 2025 AT 11:47Let’s be real. Pain is the soul screaming. Science can map the neurons, but it can’t explain why a woman in Ohio cried when she walked barefoot on grass again after 12 years. That’s not neuroplasticity. That’s grace. That’s the body remembering joy. PNE is just the dictionary entry for a miracle you didn’t know you were waiting for.
Norene Fulwiler
December 12, 2025 AT 05:04In my village in rural India, we’ve always known pain isn’t just about the body. We say: "The mind carries the ache." We don’t have scans or therapists. We have tea, silence, and someone to sit with you. This post? It’s just Western science catching up to what grandmothers knew all along.
Ada Maklagina
December 13, 2025 AT 01:48I tried PNE. Read the book. Watched the video. Did the walks. Still hurts. But now I don’t panic when it does. That’s something. Not everything. But something.
James Moore
December 14, 2025 AT 01:46I’ve been studying neurophenomenology for over a decade, and I must say - the reduction of chronic pain to a mere "volume knob" metaphor is not only oversimplified, but epistemologically negligent. The somatosensory cortex, the anterior cingulate, the insular activation - these are not whimsical dials to be turned by affirmations and YouTube videos. This is a systemic dysregulation of descending inhibitory pathways, compounded by psychosocial stressors, immune activation, and epigenetic modulation - none of which are addressed by a 30-minute conversation about smoke alarms. The clinical efficacy cited is statistically marginal and confounded by placebo effects and regression to the mean. And yet, the narrative is so seductive - because it absolves us of the terrifying truth: some pain has no solution. Only management. And management is not healing.
Kylee Gregory
December 14, 2025 AT 06:32I think the most powerful part of this isn’t the science - it’s the permission. Permission to move even when it hurts. Permission to not be broken. Permission to trust your body again. I used to think I had to earn the right to feel better. Turns out, I just had to stop fighting myself.
Lynette Myles
December 16, 2025 AT 03:59This is all part of the pharmaceutical agenda. They don’t want you to know that chronic pain is caused by 5G radiation, glyphosate in your food, and fluoride in the water. PNE is a distraction. The real cause? The government and big pharma are poisoning us. Your "volume knob" is being turned up by toxins. Your scan is normal because they wiped the data. Read the studies - they’re funded by drug companies. Don’t be fooled.
Katie Allan
December 16, 2025 AT 18:04I’ve worked with chronic pain patients for 18 years. The ones who heal aren’t the ones who got the best scans or the strongest meds. They’re the ones who stopped seeing pain as their enemy and started seeing it as a messenger. Not a villain. A teacher. PNE isn’t about fixing the body. It’s about coming home to it.