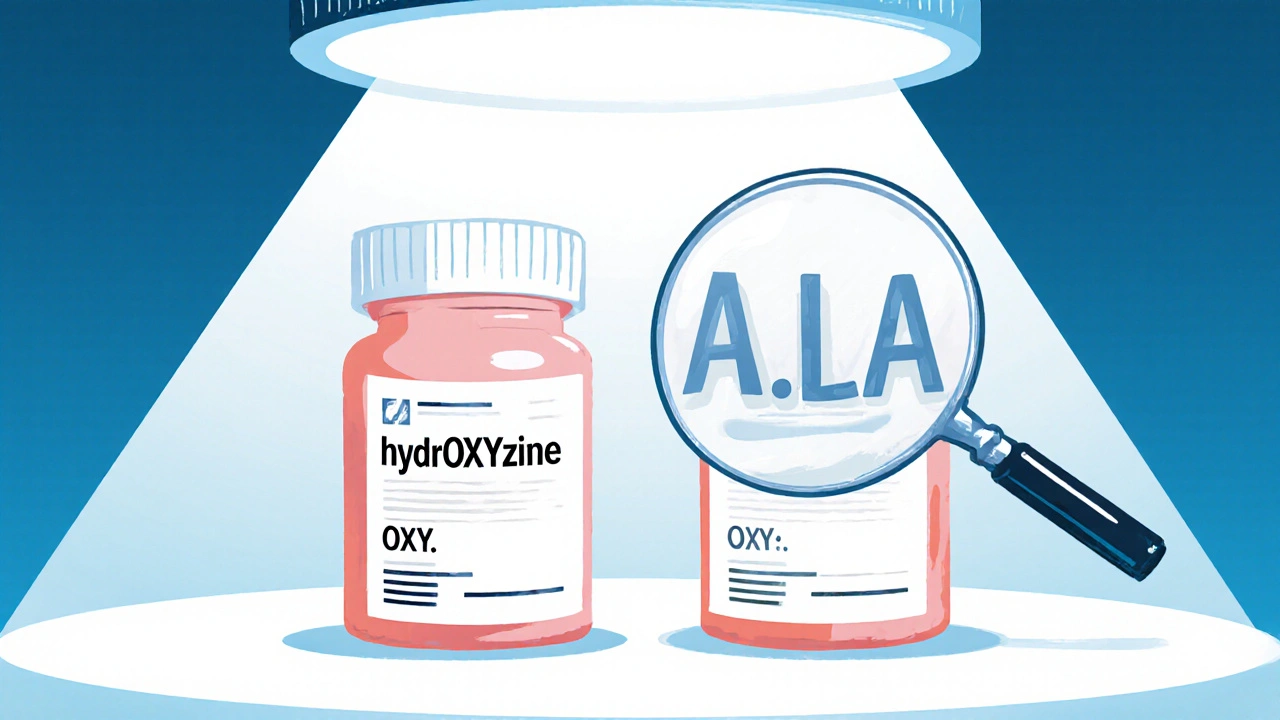
Every year, thousands of patients in the U.S. and UK receive the wrong medication-not because of a mistake in dosage, but because two drug names look or sound too similar. Look-alike and sound-alike (LASA) drug names are one of the most dangerous, yet overlooked, risks in healthcare. A patient meant to get hydralazine for high blood pressure might end up with hydroxyzine, an antihistamine used for allergies. The difference? Just a few letters. And in a busy hospital or pharmacy, those letters can disappear in a blur.
These errors aren’t rare. Studies show that about 1 in 1,000 prescriptions involves a LASA mix-up. Of those, more than one-third reach the patient, and nearly 1 in 15 causes real harm-like falls, allergic reactions, or even heart problems. The problem isn’t just handwritten scripts or tired staff. It’s built into the system. Drug names are often created without enough thought to how they’ll be confused in real-world settings.
What Is Tall Man Lettering-and Why Does It Matter?
The most common tool to fight LASA errors is called tall man lettering. It’s simple: capitalize the parts of drug names that differ. So instead of writing hydroxyzine and hydralazine, you write hydrOXYzine and hydrALAzine. The capital letters act like visual signposts, forcing your eyes to pause and compare.
The FDA started pushing for this in 2001 after a string of deadly mix-ups. Today, 35 drug pairs are officially recommended for tall man lettering, including:
- doXEPamine vs. doBUTamine
- CISplatin vs. CARBOplatin
- vinBLAStine vs. vinCRIStine
- INSULIN lispro vs. INSULIN glargine
It’s not just about capitalization. The FDA recommends capitalizing 2-4 letters that create the clearest visual contrast. Too few, and it doesn’t help. Too many, and it looks messy. The goal is to make the difference obvious at a glance-even if you’re tired, rushed, or under bright fluorescent lights.
But here’s the catch: tall man lettering only works if it’s used everywhere. A pharmacist might see hydrOXYzine on the computer screen, but the printed label from the automated dispenser shows hydroxyzine in all lowercase. That’s when errors happen.
How to Spot LASA Names in Practice
If you’re a nurse, pharmacist, or even a caregiver helping someone manage medications, here’s how to catch these errors before they happen:
- Always read the full name-not just the first few letters. Many mix-ups happen because people skim. Valtrex and Valcyte both start with “Val,” but one treats herpes, the other a serious viral infection. The full name matters.
- Look for capital letters in electronic systems and printed labels. If you don’t see them, ask why. Many older printers or EHR systems don’t apply tall man lettering automatically.
- Compare brand and generic names. For example, Valtrex is the brand name for valacyclovir, and Valcyte is for valganciclovir. Seeing both names together reduces confusion by over half, according to ECRI Institute data.
- Check the purpose. Is this medication for pain, infection, or heart failure? If the reason doesn’t match the drug, pause. A 2022 study found that adding the purpose (e.g., “for shingles”) to the label cuts errors by nearly 60%.
- Use the 3-step rule: Read the label when you pick it up, read it again when you hand it off, and read it one more time before giving it to the patient. This simple habit reduces errors by more than half.

Why Technology Alone Isn’t Enough
You might think barcode scanning or computer alerts would solve this. They help-but they’re not foolproof.
Barcode scanning prevents 89% of errors when used correctly. But it requires training, working scanners, and staff who don’t bypass the system because it’s “too slow.” One nurse in Birmingham told me she once scanned the wrong vial because the barcode was smudged-and the system didn’t flag it.
Computer alerts? They’re loud. Too loud. Clinicians override nearly half of all LASA alerts because they get flooded with them. If every alert is about a low-risk pair, people stop paying attention. The fix? Only trigger alerts for the FDA’s top 35 high-risk pairs.
And don’t forget handwritten prescriptions. In 2023, 41% of LASA errors still came from doctors scribbling names by hand. No tall man lettering there. No barcode. Just a messy “C” that could be a “D.” That’s why many hospitals now require electronic prescribing for high-risk drugs.
What’s Being Done to Fix This?
There’s real progress. The FDA added 12 new drug pairs to its tall man lettering list in September 2023. That brings the total to 35. By December 2024, all U.S. healthcare systems must use these standardized formats.
Hospitals like Johns Hopkins cut LASA errors by 67% in two years by combining:
- Tall man lettering on all screens and labels
- Forcing staff to write the treatment purpose on every order
- Setting up alerts only for the most dangerous pairs
Even the way drugs are named now has changed. Since 2018, every new drug application must pass a computer analysis using two tools: BI-SIM (for visual similarity) and ALINE (for sound similarity). These tools are 92% accurate at predicting confusion-far better than older methods. Between 2018 and 2023, 17 drug names were blocked from entering the market because they were too likely to be confused.
And now, AI is stepping in. Google Health’s Med-PaLM 2 can predict which drug names might be mixed up with 89% accuracy. It’s not replacing humans-but it’s helping designers build safer systems.
What You Can Do Right Now
You don’t need a hospital system upgrade to protect yourself or someone you care for. Here’s what you can do today:
- Ask for the generic name. If your doctor says “I’m prescribing Valtrex,” ask, “Is that valacyclovir?” Write it down.
- Check the label before taking any pill. Compare it to the prescription slip. If the name looks too similar to another drug you take, pause.
- Use a pill organizer with labels. Don’t rely on color or shape. Write the full name and purpose on each compartment.
- Speak up. If you see a label without tall man letters, or if the name looks confusing, say something. Pharmacists and nurses want to hear it.
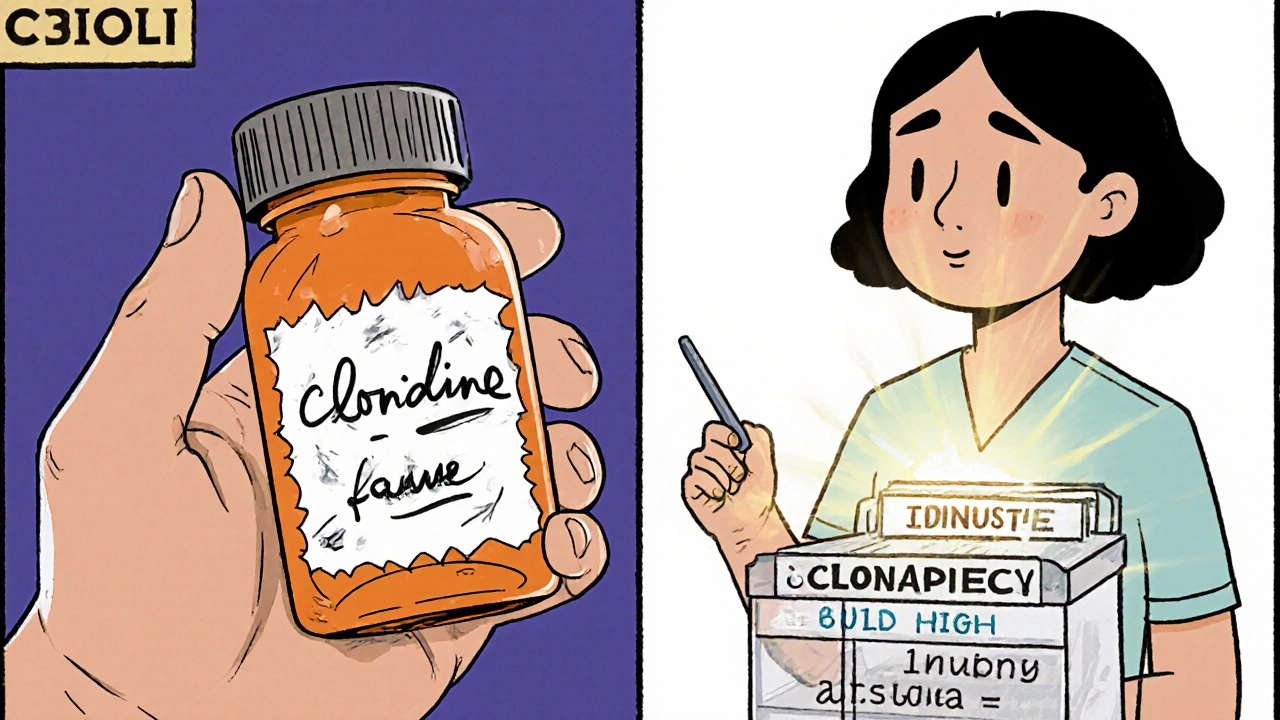
One pharmacist in Leeds told me she started asking patients, “Have you ever taken this before?” and “What’s this for?” after a near-miss with clonidine and clonazepam. She hasn’t had another error since.
Final Thought: Safety Is a Habit, Not a Feature
Tall man lettering, barcodes, and alerts are tools. But they only work if people use them right. The biggest danger isn’t bad design-it’s complacency. When you think, “It’s probably fine,” or “I’ve seen this before,” that’s when mistakes happen.
Medication safety isn’t about having the latest tech. It’s about slowing down, reading carefully, and trusting your gut when something looks off. Because in healthcare, a single letter can change everything.
What are the most common look-alike drug name pairs?
The most common and dangerous pairs include: hydrOXYzine vs. hydrALAzine, doXEPamine vs. doBUTamine, vinBLAStine vs. vinCRIStine, CISplatin vs. CARBOplatin, and INSULIN lispro vs. INSULIN glargine. These are officially listed by the FDA for tall man lettering. Other frequent pairs include clonIDINE vs. clonAZepam and epINEPHrine vs. epINEPHrine (same spelling, different concentrations).
Does tall man lettering really work?
Yes-but only when used consistently. Studies show tall man lettering reduces visual confusion errors by about 32%. When combined with color coding and purpose-of-treatment labels, effectiveness jumps to 59%. However, if it’s only applied in one system (like the EHR) and not on printed labels or automated dispensers, errors still happen. Consistency across all touchpoints is key.
Why aren’t all drug names changed to avoid confusion?
Changing drug names is extremely difficult. Once a drug is on the market, changing its name affects everything: prescriptions, insurance codes, packaging, databases, and patient records. It’s expensive and disruptive. Instead, regulators focus on identifying high-risk pairs and using tall man lettering as a visual fix. New drugs now go through strict screening to avoid confusion before they’re even approved.
Can smartphone apps help identify look-alike names?
Yes. Pilot programs at Mayo Clinic and other hospitals have tested apps that use camera recognition to scan pill bottles or vials and compare them against a database of known LASA pairs. These tools have shown 94% accuracy in identifying potential mix-ups. While not yet widely available to the public, some pharmacy apps now include LASA warnings when you search for a medication.
What should I do if I suspect a LASA error?
Stop. Don’t take the medication. Double-check the prescription against the label. If it still looks wrong, ask the pharmacist to verify the drug and its purpose. If you’re a healthcare worker, report the near-miss through your facility’s safety system. Reporting these events-even if no harm occurred-is how systems improve. The FDA and ISMP track these reports to update their lists and warnings.

Comments (14)
Lisa Detanna
November 21, 2025 AT 14:25As a nurse in Chicago, I’ve seen hydralazine swapped for hydroxyzine more times than I can count. The worst part? It’s always the tired night shift. Tall man lettering helps, but only if the pharmacy’s printer actually uses it. We had to manually highlight the caps on printouts for months. It’s not ideal, but it saved a patient last year. Just don’t trust the machines.
Demi-Louise Brown
November 21, 2025 AT 14:34Tall man lettering is a necessary tool but not a complete solution. Consistency across all platforms-EHR, printed labels, automated dispensers-is non-negotiable. Without it, visual cues become meaningless.
Matthew Mahar
November 22, 2025 AT 21:09yo i just saw a label that said 'hydrOXYzine' but the bottle said 'hydroxyzine' and i was like... are we still doing this in 2025?? like come on. one letter. one. and people die. i swear if my grandma gets the wrong pill i'm gonna storm the pharmacy with a megaphone
John Mackaill
November 23, 2025 AT 14:34I’ve worked in UK pharmacies for 18 years. The real issue isn’t just the names-it’s the lack of training. Staff are rushed, systems are fragmented, and no one checks the purpose. I started writing ‘for anxiety’ or ‘for BP’ beside every LASA pair. It’s simple, and it cuts errors. No tech needed.
Adrian Rios
November 23, 2025 AT 16:46Let’s be real-this isn’t just about capital letters. It’s about a healthcare system that treats safety like an afterthought. We’ve got AI models that can predict confusion with 89% accuracy, but hospitals still use outdated printers that can’t even render uppercase O’s properly. And don’t get me started on handwritten scripts. One doctor wrote ‘clonidin’ instead of ‘clonidine’ and the pharmacist just assumed it was a typo. That’s not diligence, that’s negligence wrapped in a white coat. We need mandatory training, standardized formatting across ALL platforms, and consequences when people cut corners. This isn’t rocket science. It’s basic human care.
Casper van Hoof
November 24, 2025 AT 07:10The structural irony lies in the fact that we engineer pharmaceutical nomenclature with scientific precision, yet permit orthographic ambiguity to persist as a systemic vulnerability. The solution is not merely typographic, but epistemological: we must reconceptualize drug identification not as a linguistic exercise, but as a cognitive safety protocol.
Ragini Sharma
November 25, 2025 AT 22:41so i just googled 'doxepamine vs dobutamine' and my phone autocorrected 'doxepine'... and i was like... yep. we're all gonna die. also why is insuline lispro capitalized but not the other one? this is chaos.
Linda Rosie
November 27, 2025 AT 02:33Read the label. Twice.
Vivian C Martinez
November 28, 2025 AT 23:32My mom used to mix up clonidine and clonazepam until I started printing out the purpose next to every pill on her organizer. Now she says, ‘I don’t take the sleepy one unless I’m having panic attacks.’ Simple. Effective. No tech required. Just care.
Ross Ruprecht
November 30, 2025 AT 07:15Why are we even talking about this? Just make all the names sound like ‘Xylophane-7B’ and be done with it. Nobody remembers them anyway.
Bryson Carroll
November 30, 2025 AT 14:39People keep acting like this is a new problem. It’s not. It’s the same arrogance that let them brand a drug ‘Zyprexa’ and then act shocked when someone misreads it as ‘Zyprexa’ (same spelling, different dose). We don’t need tall man letters-we need to stop letting pharmaceutical companies name drugs like they’re trying to sell energy drinks.
Jennifer Shannon
December 1, 2025 AT 11:38I’ve been a caregiver for my dad since his stroke, and I can tell you-this isn’t just about hospitals. It’s about families. I keep a little notebook now: drug name, generic name, purpose, color, shape, and the scribbled note from the pharmacist. I read it aloud to him every time he takes a pill. Sometimes he forgets. Sometimes I forget. But we never skip the read-aloud. It’s our ritual. And yeah, I’ve caught two mistakes already-one because the label said ‘insulin glargine’ without the caps, and another because the pill was the wrong shade of blue. No one else noticed. But we did. Because we slow down. Because we care. And honestly? That’s the only tech that’s ever saved us.
Suzan Wanjiru
December 3, 2025 AT 01:56Just had a patient bring in a bottle labeled 'vinCRIStine' but the script said 'vinBLAStine'. I checked the EHR-both were correct. The dispenser printed lowercase. I flagged it. They fixed it. But why does this still happen? We have the tools. We just don't use them right.
Kezia Katherine Lewis
December 3, 2025 AT 02:05The implementation of tall man lettering represents a low-cost, high-yield intervention within the broader framework of pharmacovigilance. However, its efficacy is contingent upon adherence to standardized nomenclature protocols across the medication use process-prescribing, dispensing, and administration. Without interoperability between EHRs, pharmacy automation systems, and label-printing technologies, the intervention remains a fragmented mitigation strategy rather than a systemic solution.