Benign Prostatic Hyperplasia is a non‑cancerous enlargement of the prostate gland that commonly causes urinary obstruction in men over 50. When the prostate swells, it compresses the urethra, leading to a cascade of lower urinary tract issues. At the same time, another chronic pelvic condition-Interstitial Cystitis-emerges as a painful bladder syndrome without infection. Although they affect different organs, the two disorders often intersect, leaving patients with overlapping, confusing symptoms.
Why the Two Conditions Overlap
Both Benign Prostatic Hyperplasia and Interstitial Cystitis belong to a broader group called Lower Urinary Tract Symptoms (LUTS). LUTS includes urgency, frequency, nocturia, weak stream, and incomplete emptying. Because the prostate sits just below the bladder, its enlargement can irritate the bladder wall, while chronic bladder inflammation in IC can increase pelvic floor tension, squeezing the prostate. Studies from urological societies (e.g., European Association of Urology, 2023) report that up to 30% of men with BPH also meet IC diagnostic criteria.
Key Anatomical Players
The Prostate is a walnut‑sized gland surrounding the urethra, responsible for producing seminal fluid. Its growth is driven by hormonal changes, particularly dihydrotestosterone. The Bladder stores urine and coordinates voiding through the detrusor muscle. In Interstitial Cystitis, the bladder lining becomes leaky, exposing underlying nerves to irritating substances, which triggers pain and urgency. When BPH compresses the urethra, the bladder must work harder, potentially aggravating the fragile bladder lining.
Shared Symptom Profile
Patients often report a confusing mix of:
- Frequent daytime urination (≥8 times)
- Nocturia (waking ≥2 times per night)
- Urgency with or without pain
- Weak or intermittent stream
- Pelvic pressure or burning sensation
Because the symptom list mirrors that of Overactive Bladder, clinicians must tease out the root cause using targeted tests.
Diagnostic Pathway: Untangling the Knot
1. History & Physical Exam: A detailed timeline helps spot whether urinary trouble started gradually (typical BPH) or abruptly with pelvic pain (suggestive of IC).
2. Urodynamic Studies: Measure bladder pressure during filling and voiding. BPH shows obstructive flow patterns; IC reveals low‑capacity, high‑sensitivity bladder.
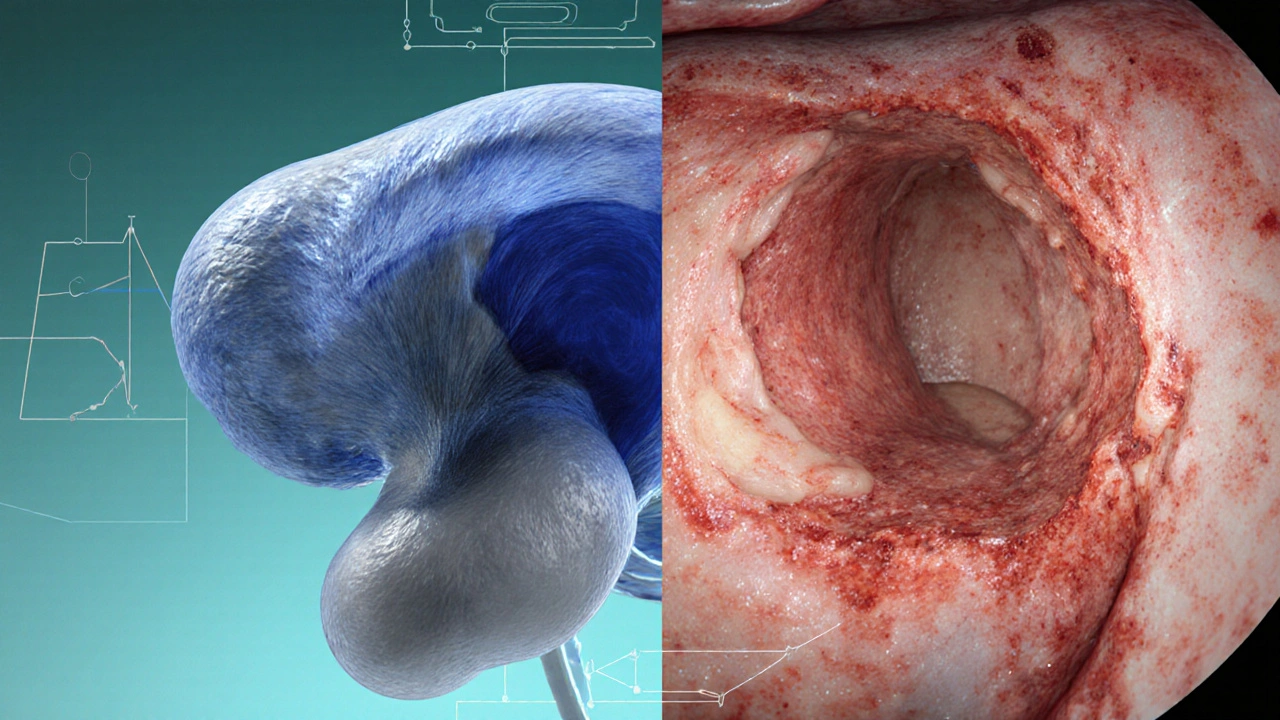
3. Cystoscopy: Direct visualization can spot glomerulations or Hunner lesions (IC markers) and assess prostate protrusion into the bladder neck.
4. Pelvic Floor Evaluation: Dysfunction here may amplify both disorders, so a physiotherapist may perform manual testing.
5. Laboratory tests: Rule out infection, PSA levels for prostate health, and urine cytology to exclude cancer.
Treatment Strategies: One Size Does Not Fit All
Because BPH and IC can feed each other, a dual‑approach often works best.
Medications Targeting the Prostate
Alpha‑blockers (e.g., tamsulosin) relax smooth muscle in the prostate and bladder neck, improving flow. 5‑alpha reductase inhibitors (e.g., finasteride) shrink prostate size over months by blocking hormone conversion. Both classes reduce obstructive LUTS but can sometimes worsen bladder pain if IC is dominant.
Therapies Aimed at Interstitial Cystitis
First‑line includes oral pentosan polysulfate, intravesical dimethyl sulfoxide (DMSO) instillations, and bladder‑protective diets (low‑acid, low‑caffeine). Physical therapy focusing on pelvic floor release can lower pressure on both bladder and prostate. For refractory cases, neuromodulation (e.g., sacral nerve stimulation) helps reset abnormal bladder signaling.
Combined or Sequential Plans
Clinicians often start with alpha‑blockers to ease obstruction, then add IC‑specific meds once urinary flow improves. If pain persists, a low‑dose regimen of both drug classes can be tried, monitoring for side‑effects such as hypotension or sexual dysfunction.
Comparison of BPH vs. IC
| Aspect | Benign Prostatic Hyperplasia | Interstitial Cystitis |
|---|---|---|
| Primary organ | Prostate gland | Bladder wall |
| Typical age | 50‑80 years | 30‑60 years (female > male) |
| Core symptom | Weak stream / incomplete emptying | Painful urgency |
| Diagnostic hallmark | Enlarged prostate on ultrasound | Glomerulations / Hunner lesions on cystoscopy |
| First‑line meds | Alpha‑blockers, 5‑alpha reductase inhibitors | Pentosan polysulfate, bladder instillations |
| Response to antibiotics | Usually none | Rarely effective |
Living with Co‑existing BPH and IC: Practical Tips
Stay hydrated, but sip slowly. Large volumes trigger urgency; small, frequent drinks keep the bladder calm.
- Schedule bathroom trips every 2‑3hours to avoid panic‑driven over‑filling.
- Warm baths or heating pads can relax the pelvic floor, reducing both urinary resistance and bladder pain.
- Track symptoms in a diary; note medication timing, diet, and stress levels.
- Consider a low‑oxalate, low‑spice diet; many IC patients report fewer flare‑ups.
- Regular follow‑up with a urologist who understands the overlap is crucial.
Future Directions: Research and Emerging Therapies
Recent trials (2024) explore combined alpha‑blocker and neuromodulation protocols, showing a 22% improvement in quality‑of‑life scores for men with both conditions. Stem‑cell injections into the bladder submucosa are also under investigation for restoring the glycosaminoglycan layer, potentially easing IC while not affecting prostate size. Personalized genomics may soon predict which men are prone to the dual pathology, paving the way for early lifestyle interventions.

Frequently Asked Questions
Can Benign Prostatic Hyperplasia cause Interstitial Cystitis?
BPH itself does not directly create IC, but the chronic urethral obstruction can irritate the bladder wall and trigger inflammation that mimics IC. In many cases, the two conditions develop independently but exacerbate each other.
What tests differentiate BPH from IC?
Urodynamic studies, prostate ultrasound, and cystoscopy are the main tools. BPH shows an enlarged prostate and obstructive flow rates, while IC reveals bladder capacity <200ml, glomerulations, or Hunner lesions on cystoscopy.
Are the medications for BPH safe for someone with IC?
Alpha‑blockers are generally well‑tolerated and can even lessen bladder outlet pressure, helping IC symptoms. However, 5‑alpha reductase inhibitors may cause sexual side‑effects that could increase pelvic floor tension, potentially worsening pain. Always discuss with a urologist.
Can lifestyle changes improve both conditions?
Yes. Reducing caffeine, alcohol, and acidic foods helps IC, while maintaining a healthy weight and regular exercise can lower prostate‑enlargement risk. Pelvic floor physical therapy is a shared benefit for both.
What is the outlook for men dealing with both BPH and IC?
With a tailored treatment plan-combining medication, bladder‑protective strategies, and pelvic‑floor therapy-most men achieve significant symptom relief. Ongoing research promises even better options as we understand the prostate‑bladder cross‑talk more clearly.


Comments (17)
RONEY AHAMED
September 27, 2025 AT 20:38Great rundown on how BPH and IC can play off each other. Keeping an eye on both symptoms can save a lot of hassle later.
emma but call me ulfi
September 28, 2025 AT 02:11Managing fluid intake in small sips really helps avoid sudden urgency spikes.
Alyssa Matarum
September 28, 2025 AT 07:44Alpha‑blockers relax prostate muscles, while pentosan protects the bladder lining.
Lydia Conier
September 28, 2025 AT 13:18Managing patients with both BPH and IC can be a real juggling act. First, it’s essential to get a thorough history that separates obstructive symptoms from painful urgency. Second, a urodynamic study helps pinpoint whether the bladder is over‑active because of obstruction or due to inflammation. Third, imaging the prostate with ultrasound confirms the size and rule out other pathologies. Fourth, cystoscopy can reveal Hunner’s lesions that are a hallmark of IC. Fifth, pelvic floor assessment should not be skipped because tight muscles can worsen both conditions. Sixth, starting with an alpha‑blocker often provides quick relief of flow issues. Seventh, once the flow improves, adding a bladder protective agent like pentosan polysulfate can address the pain component. Eighth, diet modifications-cutting out caffeine, acidic foods, and spicy meals-help many patients find calmer days. Ninth, regular bladder training and timed voiding can reduce frequency spikes. Tenth, physical therapy focused on the pelvic floor can release tension that otherwise compresses the prostate. Eleventh, for refractory cases, neuromodulation offers a promising avenue, though insurance coverage can be a hurdle. Twelfth, monitoring side‑effects such as hypotension from alpha‑blockers or sexual dysfunction from 5‑alpha reductase inhibitors is crucial. Thirteenth, patient education about the overlapping nature of LUTS empowers them to report subtle changes early. Fourteenth, a multidisciplinary team-urologist, pelvic floor therapist, and pain specialist-often yields the best outcomes. Fifteenth, follow‑up appointments every three to six months keep the treatment plan on track and allow adjustments as needed. Finally, keep an eye on emerging research, because new combination therapies are constantly being tested and could become the new standard of care.
ruth purizaca
September 28, 2025 AT 18:51Interesting read, though the depth is somewhat lacking.
Shelley Beneteau
September 29, 2025 AT 00:24I wonder how often urologists coordinate with pelvic floor therapists when both BPH and IC present; multidisciplinary care seems key.
Sonya Postnikova
September 29, 2025 AT 05:58Love the balanced approach 😊! Taking meds step‑by‑step makes the whole process less overwhelming.
Anna Zawierucha
September 29, 2025 AT 11:31Oh sure, because juggling pills is exactly what my weekend was missing – thanks for the “help”.
Mary Akerstrom
September 29, 2025 AT 17:04Sounds like staying hydrated and tracking symptoms can really make a difference.
Delilah Allen
September 29, 2025 AT 22:38Indeed, the interplay between BPH and IC is complex; however, many clinicians overlook the pelvic floor-this oversight is unacceptable; we must demand comprehensive evaluations!
Nancy Lee Bush
September 30, 2025 AT 04:11Excellent summary! The emerging stem‑cell research is especially promising-looking forward to seeing real‑world results soon! 😊
Dan Worona
September 30, 2025 AT 09:44Sure, but keep an eye on the pharma companies pushing those “new” therapies-they’re often more about profit than patient care.
Howard Mcintosh
September 30, 2025 AT 15:18Gotta say, the combo of alpha‑blockers + neuromodulation sounds like a game‑changer, even if the name feels like sci‑fi.
Jeremy Laporte
September 30, 2025 AT 20:51Totally agree, its like getting two superpowers in one package-just hope the side‑effects stay low.
Andy Lombardozzi
October 1, 2025 AT 02:24The personalized genomics approach could revolutionize early detection and prevention strategies for co‑existing BPH and IC.
Joshua Ardoin
October 1, 2025 AT 07:58Yo, that’s lit 🚀! Imagine a future where we can tweak our DNA to dodge both problems-mind blown.
Glenn Gould
October 1, 2025 AT 13:31Can't wait to see more data on the combined protocols- they’ll probably save a ton of people from endless doctor hops.