Right now, more than 270 medications are in short supply across the United States. This isn’t a temporary hiccup-it’s a persistent crisis affecting hospitals, clinics, and patients every single day. If you or someone you know relies on chemotherapy, IV fluids, or even common antibiotics, you’re likely feeling the impact. These aren’t obscure drugs. They’re the ones doctors reach for first when treating cancer, infections, dehydration, and chronic conditions. And the list keeps growing.
What’s Actually Missing Right Now?
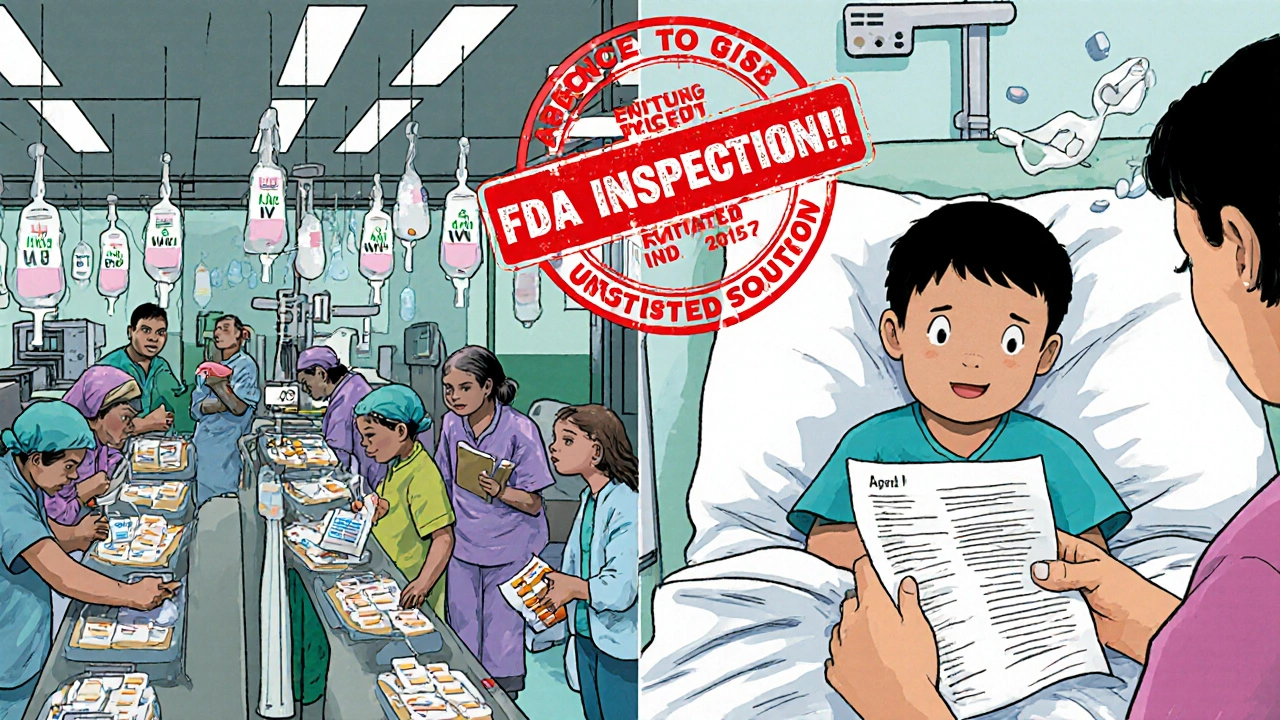
The most critical shortages are in sterile injectables-medications given directly into the bloodstream. These are hard to make, require clean-room facilities, and have razor-thin profit margins. That’s why they’re the first to vanish when supply chains stumble.
- 5% Dextrose Injection (small bags): In shortage since February 2022. Used to treat low blood sugar, dehydration, and as a carrier for other IV drugs. Expected resolution: August 18, 2025.
- 50% Dextrose Injection: Shortage since December 2021. Critical for emergency hypoglycemia. Expected resolution: September 3, 2025.
- Cisplatin: A frontline chemotherapy drug for testicular, ovarian, and lung cancers. A 2022 FDA shutdown of an Indian manufacturing plant-responsible for half the U.S. supply-left hospitals rationing doses. Some cancer centers now prioritize patients with testicular cancer, where cisplatin is most effective.
- Vancomycin: One of the last-resort antibiotics for MRSA infections. Shortages have forced providers to use older, less reliable alternatives.
- Levothyroxine: The main treatment for hypothyroidism. Demand has surged 25% since 2022, and manufacturing delays have left pharmacies scrambling.
- Epinephrine auto-injectors: Used for severe allergic reactions. Some brands are experiencing intermittent shortages, forcing patients to carry multiple types or risk being without.
It’s not just these. Saline solutions, insulin, and even common painkillers like morphine sulfate injections are hitting critical lows in certain regions. The FDA’s latest update shows 12 new shortages added in the first quarter of 2025-mostly in hormonal and central nervous system drugs.
Why Are These Shortages Happening?
It’s not one problem. It’s a chain reaction.
First, most of the raw ingredients-active pharmaceutical ingredients (APIs)-come from just two countries: India and China. About 45% of APIs come from India, 25% from China. These places make the bulk of generic drugs because they’re cheaper. But quality control issues are common. A single failed inspection at a plant in Hyderabad or Shanghai can shut down supply to the entire U.S. for months.
Second, profit margins are tiny. Generic drugs make up 90% of prescriptions but only 20% of drug spending. Manufacturers earn just 5-8% profit on generics. Compare that to brand-name drugs, which can make 30-40%. Why would a company invest in building more capacity for a low-margin product when they can make more money elsewhere?
Third, demand is exploding. ADHD medications like Adderall and Vyvanse have seen usage rise 35% since 2020. GLP-1 weight-loss drugs like Ozempic and Wegovy are in even worse shape-some pharmacies can’t get them at all. These aren’t just lifestyle drugs. Many patients depend on them for diabetes control, heart health, and metabolic disease management.
Finally, the system doesn’t see shortages coming. Manufacturers aren’t required to tell the FDA about potential disruptions until it’s too late. The FDA can warn hospitals, but it can’t force a company to produce more. In 2024, the agency prevented about 200 potential shortages-but only because they got lucky with early reports. Most of the time, they’re reacting, not preventing.
What’s Happening in Hospitals?
Behind the scenes, pharmacists are working overtime. One study found that 92% of hospital pharmacists spend more than 10 hours a week just managing shortages. That’s time they’re not spending on patient care, medication reviews, or safety checks.
Substitutions are common-but risky. A pharmacist might swap one antibiotic for another that’s slightly less effective. Or replace a saline bag with a different concentration, which can throw off electrolyte balances in critically ill patients. In 2024, 67% of hospitals reported medication errors directly tied to shortage-driven substitutions.
Doctors are forced to delay treatments. A survey by the American Medical Association found 78% of physicians had to postpone care because a needed drug wasn’t available. For cancer patients, a 14-day delay in chemotherapy can mean the difference between remission and progression.
Patients aren’t always told. Some get a different drug without knowing it’s a substitute. Others wait weeks for a refill, unsure if their condition is worsening because of the shortage-or their disease.
Who’s Getting Hit the Hardest?
It’s not evenly distributed. People on Medicaid, Medicare, or without insurance are hit hardest. They’re more likely to rely on generics, which are the most affected. Rural hospitals have fewer backup suppliers. One hospital in rural Ohio told the FDA they couldn’t get any IV fluids for two weeks in early 2025. They had to transfer patients to the nearest city 80 miles away.
Cancer patients are in a particularly brutal position. Cisplatin, carboplatin, and doxorubicin shortages mean some are getting less effective treatments-or none at all. Patients for Affordable Drugs reported that 31% of cancer patients experienced treatment interruptions in 2024. That’s nearly one in three.
Children with chronic conditions like cystic fibrosis or epilepsy are also vulnerable. Many rely on injectable antibiotics or anti-seizure meds that are now scarce. Parents are calling pharmacies daily, checking every location, just to get a 10-day supply.

What’s Being Done?
Some fixes are happening-slowly.
The FDA launched a new public reporting portal in January 2025. Healthcare providers can now report shortages that aren’t yet on the official list. In just three months, they received over 1,200 reports-and acted on 87% of them.
Forty-seven states now let pharmacists swap in similar drugs during shortages. But only 19 states allow that without a doctor’s OK. That delay can cost lives in emergencies.
New York is testing an online database that shows which pharmacies have which drugs in stock. Hawaii’s Medicaid program now allows FDA-approved drugs from other countries to be used during shortages-a controversial but practical move.
The U.S. Pharmacopeia is pushing for three big changes: financial incentives to bring API manufacturing back to the U.S., mandatory stockpiles of critical drugs, and a national early warning system that connects manufacturers, distributors, and hospitals in real time.
But without policy changes, the problem will keep getting worse. The Congressional Budget Office predicts shortages will stay above 250 through 2027. If new tariffs on Chinese and Indian pharmaceuticals go through, the number could jump to 350 or more.
What Can You Do?
If you’re on a medication that’s in short supply:
- Don’t wait until your last pill to call your pharmacy. Check early and often.
- Ask your doctor about alternatives. Sometimes there’s a different brand or formulation that works just as well.
- Keep a written list of your meds, doses, and why you take them. This helps pharmacists and doctors find substitutes faster.
- Sign up for alerts from ASHP’s Drug Shortages Database. It’s free and updated weekly.
- If you’re a caregiver for a child or elderly person, communicate with their care team regularly. Don’t assume everything is fine just because you haven’t heard otherwise.
There’s no easy fix. But awareness helps. The more people know, the more pressure there is to fix the system.
How long do drug shortages usually last?
There’s no standard timeline. Some shortages last a few weeks; others drag on for years. The average resolution time improved by 15% in 2024 due to better FDA coordination, but many of today’s shortages-like 5% Dextrose and cisplatin-have been ongoing since 2021 or earlier. Complex manufacturing issues, especially with sterile injectables, often take 6 to 18 months to resolve.
Can I get a different brand if my drug is out of stock?
Yes, in many cases. Pharmacists can substitute generic equivalents or therapeutically similar drugs if your state allows it. For example, if your brand-name levothyroxine is unavailable, a generic version may be substituted. But not all substitutions are safe-especially with narrow-therapeutic-index drugs like warfarin or lithium. Always confirm with your doctor or pharmacist that the alternative is appropriate for your condition.
Why aren’t more drugs made in the U.S.?
It’s expensive. Building a compliant manufacturing facility for sterile injectables can cost over $100 million. The U.S. market pays less for generics than Europe or Canada, so companies don’t see a return on investment. Most manufacturers choose to produce in countries where labor and regulation costs are lower-even if it means risking quality or supply chain disruptions.
Are brand-name drugs affected too?
Yes, but less often. Brand-name drugs have higher profit margins, so companies can afford to keep backup supplies or pay premium prices for ingredients. Drugs like Ozempic, Humira, and Keytruda still face shortages, but mostly due to overwhelming demand-not manufacturing failures. The real crisis is in generics, which make up the vast majority of prescriptions.
Is it safe to use a drug from another country during a shortage?
Under normal circumstances, no. But in emergencies, some states like Hawaii have temporarily allowed FDA-approved drugs from Canada, the EU, or Australia to be imported. These drugs meet the same safety standards as U.S. versions-they’re just not sold here due to pricing rules. This is a stopgap, not a long-term solution, but it’s saved lives during critical shortages.


Comments (15)
Daisy L
November 21, 2025 AT 15:40This is a national emergency-and no one’s doing anything about it! We’re letting India and China hold our medicine hostage while our politicians sip lattes and tweet about ‘supply chain resilience’!?!? We need to nationalize pharma manufacturing NOW-like, yesterday! Bring back the factories! Stop outsourcing life-saving drugs like they’re cheap T-shirts from Alibaba! I’m sick of watching my mom ration insulin because some factory in Hyderabad failed an inspection! This isn’t capitalism-it’s criminal negligence!
Anne Nylander
November 22, 2025 AT 13:11Hey everyone-just wanted to say you’re not alone. I’ve been there-waiting weeks for my kid’s seizure meds. It’s terrifying. But please don’t give up. Call your pharmacy every day. Talk to your doctor. Join the ASHP alerts. I did-and we got our refill last week! You got this. One step at a time. 💪
Franck Emma
November 23, 2025 AT 21:11My dad died because they ran out of cisplatin. They gave him a ‘substitute.’ It didn’t work. They didn’t tell us it wasn’t the same. Now I’m screaming into the void. Again.
Noah Fitzsimmons
November 25, 2025 AT 16:05Oh wow, a 270-drug shortage? Shocking. Next you’ll tell me the sun rises in the east. Did you also know that people still die from heart attacks? And that water is wet? This is like reporting that ‘cars sometimes break down.’ Groundbreaking. Also, why are you surprised? You live in a country that outsources everything and then blames the people who made it possible. Grow up.
Eliza Oakes
November 26, 2025 AT 05:30Wait-so you’re telling me the U.S. government can’t fix this? That’s hilarious. I’ve seen more reliable supply chains in my local bodega. Also, why are we still using 1970s-era drug approval systems? And why is no one talking about how Big Pharma bribes the FDA to look the other way? This isn’t a shortage-it’s a cartel. And you’re all just sitting here like it’s a TED Talk.
Clifford Temple
November 27, 2025 AT 22:03China and India are literally weaponizing our medicine. This isn’t a market failure-it’s an act of war. We need tariffs. We need military escorts for drug shipments. We need to shut down every Indian API plant until they start making quality stuff. And if they won’t? We bomb their factories. No more excuses. Our children’s lives are not negotiable.
Shawn Sakura
November 28, 2025 AT 19:19Hey, just wanted to say-this is hard, but we’re not powerless. I’m a pharmacist, and I’ve been using the FDA’s new portal to report shortages. We’re getting responses faster now. Also, if you’re on levothyroxine, try Synthroid if your generic’s out. It’s not perfect, but it’s better than nothing. And hey-you’re not crazy for feeling scared. You’re human. Keep pushing. We’re all in this together.
Paula Jane Butterfield
November 29, 2025 AT 13:25As someone who’s worked in rural clinics for 20 years, I’ve seen this coming. It’s not just about drugs-it’s about trust. Patients don’t know if they’re getting the real thing. Nurses are crying because they can’t help. We need community pharmacists to be part of the solution-not just the last line of defense. Let’s train them to be drug shortage first responders. And yes, we need more U.S. manufacturing-but also, let’s start paying pharmacists like heroes, not hourly workers.
Simone Wood
November 30, 2025 AT 18:08There’s a fundamental flaw in the entire paradigm: the assumption that healthcare is a commodity. It’s not. It’s a right. The FDA’s ‘early warning system’ is a PR stunt. Real solutions require systemic overhaul-not tinkering with databases. And the fact that Hawaii is importing drugs from Canada? That’s not innovation-that’s desperation dressed up as policy. We need a single-payer, publicly funded, domestically produced pharmaceutical infrastructure. Anything less is complicity.
Swati Jain
December 1, 2025 AT 14:06Let’s be real-this is what happens when you outsource everything and then pretend you’re a superpower. India makes 45% of the world’s generics. We’re not victims-we’re lazy. We let our own workers get paid $12/hour to make pills while CEOs in New Jersey buy yachts. Fix the pay. Fix the incentives. Stop blaming the ‘supply chain.’ It’s your own greed. And yes-I’m Indian. I’m not defending this. I’m calling it out.
Florian Moser
December 2, 2025 AT 10:32Thank you for writing this. It’s clear, detailed, and deeply human. I’ve shared it with my entire care team. We’re starting a local drug shortage awareness group-pharmacists, nurses, patients. We’re mapping which pharmacies have what, and we’re creating printed handouts for elderly patients. Small steps. But real ones. You’re not alone.
Donald Frantz
December 4, 2025 AT 06:11Has anyone checked the FDA’s new public portal? I submitted a report last week about vancomycin being unavailable in three counties. They responded within 48 hours. They’re not perfect, but they’re trying. Also-why are we not talking about the fact that insulin and epinephrine are being hoarded by middlemen? That’s a whole other layer of corruption.
Sammy Williams
December 5, 2025 AT 22:22My mom’s on levothyroxine. She’s 72. We’ve been calling 12 pharmacies a day for three weeks. Finally found a 30-day supply in a Walmart 40 miles away. We drove. It was worth it. Don’t give up. And if you’re reading this-thank you for caring. That’s half the battle.
Erika Sta. Maria
December 6, 2025 AT 10:10Oh, so now we’re blaming China? Funny. The same China that gave us the iPhone, the solar panel, and the cure for hepatitis C. But when it comes to medicine, suddenly it’s ‘evil empire’? Let’s not pretend this is about nationalism-it’s about profit. And the real villain? The shareholders who demand quarterly returns while people die waiting for saline bags. Capitalism doesn’t care if you’re alive. It only cares if you’re profitable.
Nikhil Purohit
December 7, 2025 AT 04:09As someone who’s worked in Indian API manufacturing, I can say this: quality isn’t the issue-it’s scale and cost. The U.S. pays $0.02 per pill for generic antibiotics. In Europe, it’s $0.10. That’s why factories here don’t invest in upgrades. We need fair pricing-not nationalism. And yes, we need U.S. capacity. But it’s not about ‘making America great again.’ It’s about making life sustainable for everyone.