GLP-1 Weight Loss Calculator
How This Calculator Works
Based on clinical trial data: Semaglutide (Wegovy) users lose an average of 15% of body weight over 68 weeks. Tirzepatide (Zepbound) shows even greater results. This calculator estimates your potential weight loss based on these studies. Remember: individual results vary significantly.
Your Estimated Results
Initial Weight
0 lbs
Weight Loss
0 lbs
Final Weight
0 lbs
Note: Actual weight loss may vary significantly based on individual factors, diet, exercise, and other health conditions. Results are based on clinical trial data for semaglutide (Wegovy) where users lost an average of 15% of body weight over 68 weeks.
Timeline of Results:
For years, people with type 2 diabetes were told to lose weight to manage their condition. But what if the medicine itself could help them lose weight-without extra dieting or gym sessions? That’s exactly what GLP-1 agonists are doing. Originally designed to control blood sugar, these drugs are now at the center of a revolution in weight loss treatment. And it’s not just about looking different-it’s about feeling better, moving easier, and reducing the risk of heart disease, stroke, and even depression.
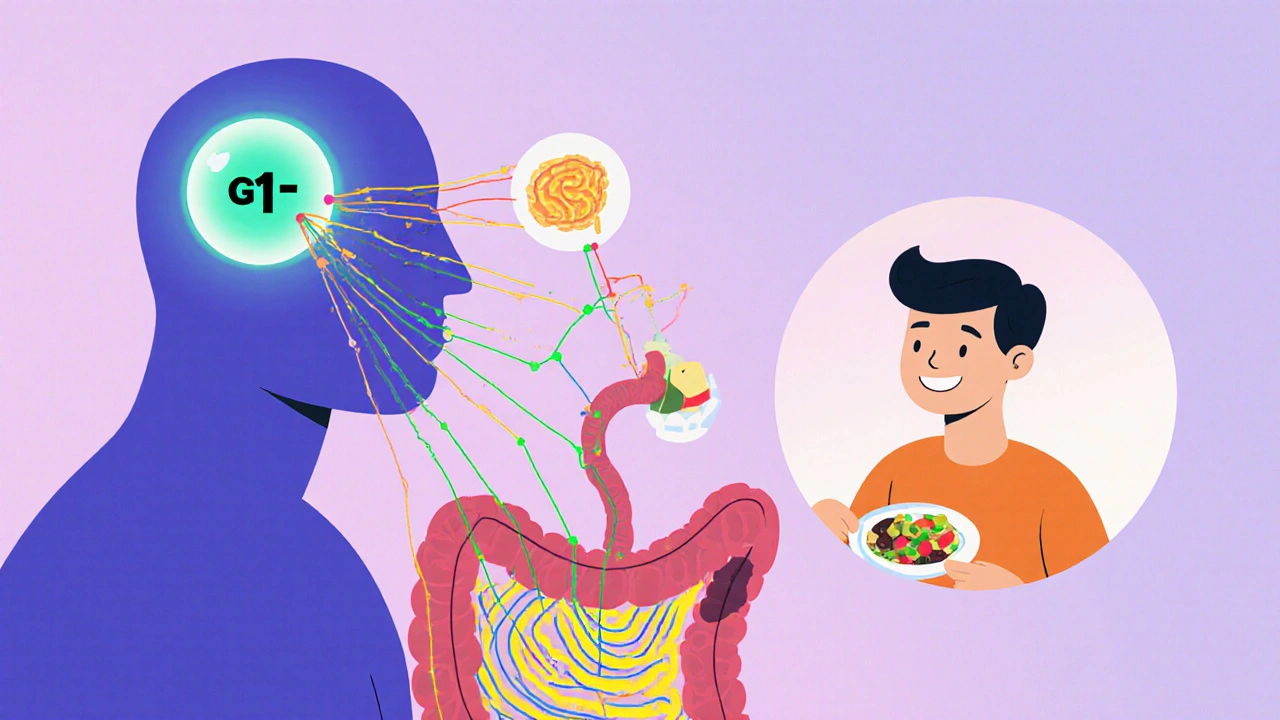
How GLP-1 Agonists Actually Work
GLP-1 agonists mimic a hormone your body already makes called glucagon-like peptide-1. This hormone does three key things: it tells your pancreas to release insulin when your blood sugar rises, it stops your liver from dumping out too much glucose, and it slows down how fast food leaves your stomach. But the biggest surprise? It also talks directly to your brain.
When you take a GLP-1 agonist like semaglutide (Wegovy) or tirzepatide (Zepbound), you don’t just feel full faster-you start craving less food overall. Studies show people on these drugs report a dramatic drop in hunger, especially for sugary or fatty foods. That’s not just willpower. It’s biology changing.
And it’s not magic. The science is clear: these drugs reduce appetite by acting on receptors in the hypothalamus, the part of your brain that controls hunger and energy balance. They also delay gastric emptying, so meals stick around longer, keeping you satisfied. No guesswork. No calorie counting. Just a natural shift in how your body tells you when to eat-and when to stop.
Weight Loss That Actually Sticks (For a While)
Let’s talk numbers. In clinical trials, people taking semaglutide 2.4 mg weekly lost an average of 15% of their body weight over 68 weeks. That’s not a few pounds. For someone weighing 200 pounds, that’s 30 pounds gone. Tirzepatide, a newer dual-acting drug, did even better: nearly 60% of users lost 20% or more of their body weight. That’s more than most bariatric surgeries achieve.
And it’s not just for people with diabetes. The STEP-1 trial showed that even people without type 2 diabetes lost nearly 15% of their weight on semaglutide, compared to just 2.4% on placebo. That’s a 12.5-percentage-point gap-huge in medicine.
But here’s the catch: weight comes back if you stop. Clinical data shows that within a year of stopping these drugs, most people regain 50% to 70% of the lost weight. That’s why doctors now say: this isn’t a quick fix. It’s a long-term tool. Like blood pressure meds or insulin, you might need to stay on it to keep the benefits.
Beyond the Scale: Heart, Brain, and More
Weight loss is the headline. But the real value might be what happens underneath.
GLP-1 agonists lower blood pressure. They improve cholesterol-raising good HDL and lowering bad triglycerides. They reduce inflammation markers linked to heart disease. A 2024 study from the University of Chicago found these drugs cut the risk of heart attacks, strokes, and heart-related deaths by up to 18% in people with existing heart conditions.
And then there’s the brain. A 2024 study of over 2 million U.S. veterans found people on GLP-1 agonists had a 23% lower risk of seizures, a 17% lower risk of substance use disorders (including alcohol and opioids), and a 14% lower rate of suicidal thoughts. That’s not something you see with other weight loss drugs. It suggests these medications might be doing more than just shrinking fat-they might be calming an overactive stress response or stabilizing brain chemistry.
Even more surprising? A 2024 study linked GLP-1 use to a 16% lower risk of bulimia and an 11% lower risk of schizophrenia. Researchers are still figuring out why. But if true, this could open the door to treating mental health conditions with metabolic drugs.

Side Effects: Nausea, Cost, and ‘Ozempic Face’
It’s not all smooth sailing.
Nausea is the most common side effect-reported by 20% to 30% of users. Vomiting and diarrhea happen too, especially when starting out. Most people get used to it after a few weeks, but for some, it’s enough to quit. Reddit users on r/semaglutide describe it as ‘constant nausea making work difficult’-a real barrier for people with desk jobs or busy lives.
Then there’s ‘Ozempic face.’ It’s not a medical term, but it’s real. As people lose weight rapidly, facial fat disappears. Skin can sag. Cheeks look hollow. Some people report looking older, even if they’re healthier. Harvard Health documented this in 42% of long-term users. It’s not dangerous-but it’s noticeable. And it’s irreversible without cosmetic procedures.
Cost is the biggest hurdle. Wegovy costs around $1,349 a month without insurance. Even with insurance, many plans require prior authorization, step therapy, or refuse coverage entirely. A 2024 survey found 58% of users struggled with insurance. That’s why so many people ration doses-skipping weeks or cutting doses in half-to stretch their supply. That’s dangerous. It increases side effects and reduces effectiveness.
Who Gets the Most Benefit?
These drugs aren’t for everyone.
They work best in people with obesity (BMI ≥30) or overweight with at least one weight-related condition-like high blood pressure, prediabetes, or heart disease. The American Diabetes Association now recommends them as first-line treatment for type 2 diabetes patients with obesity or cardiovascular disease.
But if you’re lean, with no metabolic issues, the risks might outweigh the benefits. A 5% weight loss in someone who’s already at a healthy weight doesn’t improve health-it might just make you look gaunt. And the side effects? Still there.
Also, don’t expect miracles if you’re not willing to make lifestyle changes. These drugs work best with nutrition counseling and movement. One study showed people who combined semaglutide with weekly coaching lost twice as much weight as those who took the drug alone.

How to Start and Stay on Track
If you’re considering GLP-1 agonists, start with your doctor. Don’t buy them online. Don’t use a friend’s prescription. These are prescription-only medications with serious risks if misused.
The standard approach is to start low. Semaglutide begins at 0.25 mg once a week, then slowly increases every four weeks over 16 to 20 weeks. This helps your body adjust and cuts down on nausea. Most people reach the full dose (2.4 mg) by month 5.
Keep a symptom journal. Note your hunger levels, side effects, sleep, and energy. That helps your doctor adjust your dose or suggest support. Many clinics now offer integrated programs-like Found or Calibrate-that bundle medication with nutrition, coaching, and mental health support for $99 to $149 a month.
Novo Nordisk’s Norditrac program helps eligible patients cover up to 75% of out-of-pocket costs for Wegovy. Check if you qualify. And if your insurance denies coverage, ask your doctor to appeal. Many approvals come on second try.
What’s Next?
The future of GLP-1 drugs is moving fast.
Oral versions are coming. Rybelsus is already available, but new pills in Phase 3 trials could deliver higher doses with better absorption. There are also long-acting implants being tested that last six to twelve months-no weekly shots.
Combination drugs are next. Triple agonists that hit GLP-1, GIP, and glucagon receptors are in development. Early results suggest even bigger weight loss-up to 25%.
And the market? It’s exploding. Global sales hit $35.7 billion in 2023. By 2030, analysts predict $100 billion. Companies like Amazon and Walmart are adding these drugs to employee health plans. Insurance coverage will likely improve-but only if demand keeps rising.
But here’s the question no one’s asking enough: Can we afford this? If 42% of U.S. adults have obesity, and only 2% are currently getting treatment, scaling up to millions of users could strain healthcare systems. And what happens when these drugs are no longer patent-protected? Will generics bring prices down-or will manufacturers keep them artificially high?
For now, GLP-1 agonists are the most effective weight loss tools we’ve ever had. They’re not perfect. They’re not cheap. But for many people, they’re life-changing.
Are GLP-1 agonists only for people with diabetes?
No. While they were first approved for type 2 diabetes, newer versions like Wegovy and Zepbound are specifically approved for chronic weight management in people without diabetes. The FDA approved Zepbound (tirzepatide) for weight loss in November 2023. Many people without diabetes are using these drugs off-label, and studies show they work just as well for weight loss in non-diabetic individuals.
How long does it take to see weight loss results?
Most people start noticing reduced hunger and slight weight loss within the first 2 to 4 weeks. Significant weight loss-5% or more of body weight-typically happens by 12 to 16 weeks. The biggest changes occur between months 6 and 12. Clinical trials show peak weight loss around 68 to 72 weeks, with most people continuing to lose slowly until they reach their plateau.
Do GLP-1 agonists cause muscle loss?
Some muscle loss can occur during rapid weight loss, but studies show GLP-1 agonists preserve more muscle than traditional dieting. In trials, about 25-30% of weight lost was fat-free mass (including muscle), compared to 40% or more with diet-only approaches. Combining the drug with strength training and adequate protein intake helps protect muscle. Most doctors recommend at least 2 days a week of resistance exercise while on these medications.
Can you drink alcohol while taking GLP-1 agonists?
Yes, but with caution. Alcohol can increase the risk of low blood sugar, especially if you have diabetes. It also worsens nausea and dehydration-two common side effects of GLP-1 drugs. Many users report feeling sick faster or more intensely when drinking. It’s best to limit alcohol, especially early in treatment. If you do drink, eat something first and stay hydrated.
What happens if you miss a dose?
If you miss a weekly dose, take it as soon as you remember, as long as it’s within 5 days. If it’s been more than 5 days, skip the missed dose and resume your regular schedule. Don’t double up. Missing doses can reduce effectiveness and may bring back hunger and cravings. For daily oral versions like Rybelsus, if you miss a dose, skip it and take the next day’s dose. Don’t take two at once.
Are there cheaper alternatives to Wegovy or Ozempic?
Currently, there are no true generic versions of semaglutide or tirzepatide. But older GLP-1 agonists like liraglutide (Saxenda) or dulaglutide (Trulicity) are sometimes less expensive, especially with insurance. Some patients use compounded versions of semaglutide, but these are not FDA-approved and carry higher safety risks. Manufacturer assistance programs (like Norditrac) and pharmacy discount cards can reduce out-of-pocket costs by up to 75% for eligible patients.
Is it safe to use GLP-1 agonists long-term?
So far, yes. The longest studies follow patients for 4 years, and no new major safety risks have emerged beyond the known side effects: nausea, vomiting, and rare cases of pancreatitis or gallbladder disease. The FDA requires ongoing monitoring for thyroid tumors in animal studies, but no link has been found in humans. Long-term use appears safe for most people, especially when monitored by a doctor. The bigger concern is whether the body adapts over time-some users report diminishing returns after 2-3 years.
Final Thoughts
GLP-1 agonists aren’t a magic pill. They’re a powerful tool-complex, expensive, and sometimes uncomfortable. But for millions of people struggling with weight, diabetes, and heart disease, they offer something rare: real, measurable health improvement. They’re changing how we think about obesity-not as a failure of willpower, but as a treatable medical condition.
The real win isn’t just the number on the scale. It’s the blood pressure dropping. The energy returning. The anxiety easing. The ability to walk up stairs without stopping. That’s the true benefit-beyond diabetes control. And for many, it’s life-changing.

Comments (11)
Matthew Karrs
November 20, 2025 AT 20:51Let’s be real - this is just Big Pharma’s way of turning obesity into a lifelong cash cow. You take the drug, you lose weight, then you’re hooked for life. And don’t even get me started on ‘Ozempic face’ - they’re selling you a cure while making you look like a ghost. Next thing you know, they’ll charge you extra to fix the hollow cheeks they created. 💸
Nosipho Mbambo
November 21, 2025 AT 06:34Wow. Just... wow. I mean, I’m from South Africa, and here, people are still struggling to get basic diabetes meds-yet in the U.S., folks are worried about ‘Ozempic face’? It’s like the first world’s problems are now aesthetic. I’m not mad, I’m just... confused. 🤔
Russ Bergeman
November 21, 2025 AT 19:3015% weight loss? That’s great. But did anyone check if it’s fat or muscle? And why is no one talking about the fact that these drugs are basically brain hijacking? You’re not losing weight-you’re being chemically reprogrammed to not want food. That’s not health. That’s chemical compliance.
Dana Oralkhan
November 23, 2025 AT 04:12For anyone considering this: please, please talk to a dietitian or a therapist first. These drugs aren’t magic-they’re a tool. And tools need context. I’ve seen people on them feel better mentally, but also feel lost when they stop because they never learned how to eat without the drug’s help. You’re not broken. You just need support-not just a shot.
Jeremy Samuel
November 24, 2025 AT 17:36GLP-1? More like GLP-1 ‘get me a new face’ 😂 I heard someone say they lost 30lbs and now their dog doesn’t recognize them. Also, ‘Ozempic face’ sounds like a bad horror movie. Next up: ‘Metformin Moustache’?
Destiny Annamaria
November 26, 2025 AT 12:23OMG I’m so here for this!! I’ve been on semaglutide for 6 months and I can finally wear jeans again!! Also, my anxiety? Gone. Like, poof. My therapist says it’s probably the weight loss + less inflammation. But honestly? I don’t care why-it works. 🙌💖
Ron and Gill Day
November 27, 2025 AT 06:00Let’s cut through the marketing fluff. These drugs are expensive, unproven long-term, and marketed to the obese like they’re defective products. If you’re a 300-lb person with no access to real nutrition education, you’re not ‘sick’-you’re a victim of a broken food system. This is just corporate band-aid medicine dressed up as science. Pathetic.
Alyssa Torres
November 29, 2025 AT 01:43My cousin started this last year. She went from crying in the grocery store because she couldn’t reach the top shelf to hiking 10 miles. She said the nausea lasted 3 weeks, then it was like a switch flipped. She still eats pizza-but now she stops when she’s full. That’s not magic. That’s her brain finally listening. 🥹
Summer Joy
November 30, 2025 AT 13:40Okay but what about the people who can’t afford it? I saw a Reddit post where someone was splitting pills and getting them from Mexico. That’s not healthcare. That’s a survival hack. And now we’re having a whole cultural moment about ‘Ozempic face’ like it’s a TikTok trend?? 😭 This is tragic. And also, kinda hilarious? 🤡
Aruna Urban Planner
December 1, 2025 AT 20:44The paradigm shift here is not pharmacological-it’s epistemological. We are transitioning from a moral model of obesity (lack of willpower) to a neuroendocrine model of metabolic dysregulation. This necessitates a reconceptualization of therapeutic goals: not weight as outcome, but homeostasis as process. The pharmaceutical industry, however, remains anchored in commodified outcomes, thereby perpetuating structural inequities in access and outcomes.
Nicole Ziegler
December 2, 2025 AT 23:33Just took my first shot. Nausea is REAL. But I ate a banana and laid down. Now I’m not hungry. Like... at all. 😴🍌