Drug Interaction Checker
Check Medication Interactions
Enter medications you're taking (prescription, OTC, or supplements). Check for known dangerous interactions based on pharmacokinetic and pharmacodynamic mechanisms.
Every year, thousands of people end up in the hospital not because their illness got worse, but because two medicines they were taking together started fighting each other. This isn’t rare. It’s happening right now, in kitchens, pharmacies, and doctor’s offices across the UK and beyond. These are drug-drug interactions - and they’re not just theoretical. They’re real, measurable, and often preventable.
What Exactly Is a Drug-Drug Interaction?
A drug-drug interaction happens when one medicine changes how another medicine works in your body. It doesn’t mean the drugs are chemically reacting like in a lab. It means one drug interferes with how the other is absorbed, processed, or acts on your cells. The result? The medicine might not work at all - or it might work too well, and that’s dangerous.
Think of it like traffic. One drug is a car trying to get to its destination (your target organ). Another drug is a roadblock, a detour, or even a speed bump. Sometimes the car gets stuck. Sometimes it goes too fast. Either way, the outcome isn’t what the driver intended.
Two Main Types: Pharmacokinetic vs. Pharmacodynamic
There are two big categories of drug interactions, and they work in completely different ways.
Pharmacokinetic interactions are about what your body does to the drug. This includes how it’s absorbed from your gut, how it travels through your blood, how your liver breaks it down, and how your kidneys flush it out. These are the most common - accounting for 70-80% of all clinically significant interactions.
Pharmacodynamic interactions are about what the drugs do to your body together. Two drugs might hit the same target - like your heart or your brain - and either amplify each other (good or bad) or cancel each other out. These are trickier to predict because they don’t always show up in blood tests.
How Your Liver Gets Involved: The CYP450 System
Your liver is the main cleanup crew for most medicines. It uses a group of enzymes called cytochrome P450 (CYP450) to break down drugs. There are several types, but five are the big players: CYP3A4, CYP2D6, CYP2C9, CYP2C19, and CYP1A2.
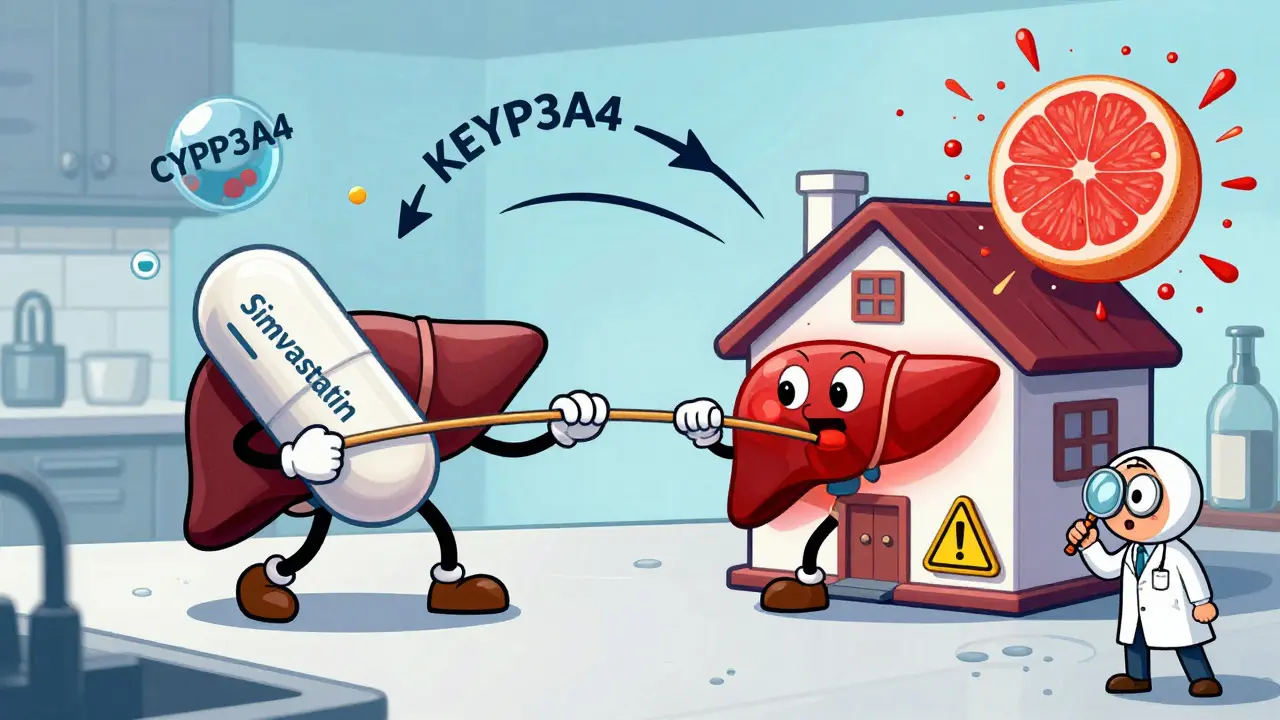
CYP3A4 alone handles about half of all prescription drugs. That includes statins like simvastatin, blood thinners like warfarin, and even some antidepressants. When something blocks or speeds up CYP3A4, the effects can be dramatic.
Take ketoconazole, an antifungal. It’s a strong CYP3A4 inhibitor. When taken with simvastatin, it can cause simvastatin levels to spike 10 to 20 times higher than normal. That’s not a little bump. That’s a red flag for rhabdomyolysis - a condition where muscle tissue breaks down and can lead to kidney failure.
On the flip side, St. John’s Wort, a popular herbal supplement for mild depression, is a CYP3A4 inducer. It tells your liver to make more of the enzyme. That means drugs like cyclosporine (used after organ transplants) get broken down too fast. In some cases, cyclosporine levels drop by 50-60%, putting the transplant at risk of rejection.
Transporters: The Hidden Gatekeepers
It’s not just the liver. Your body has tiny transport proteins that move drugs in and out of cells. One of the most important is P-glycoprotein (P-gp). It acts like a bouncer at the door of your brain, kidneys, and intestines - deciding what gets in and what gets kicked out.
Verapamil, a heart medication, blocks P-gp. When taken with digoxin - a drug used for irregular heartbeats - it stops digoxin from being flushed out of your body. Result? Digoxin builds up. Too much can cause dangerous heart rhythms. In fact, digoxin levels can jump by 50-100% with this combo.
Another transporter, OATP1B1, moves statins into the liver. If a drug like gemfibrozil blocks it, the statin stays in your blood longer. That’s why combining gemfibrozil with rosuvastatin increases the risk of muscle damage - so much so that this combo is now avoided entirely in clinical practice.
When Drugs Team Up (or Fight)
Pharmacodynamic interactions don’t change drug levels - they change what the drugs do to your body.
Take blood thinners. Warfarin and aspirin both prevent clots. But together? They can turn a small cut into a serious bleed. Studies show the risk of major bleeding jumps 3-5 times when NSAIDs like ibuprofen are added to warfarin.
Or consider QT prolongation. Certain antibiotics (like azithromycin) and fluoroquinolones (like ciprofloxacin) can slightly lengthen the heart’s electrical cycle. Alone, it’s usually harmless. Together? The risk of a life-threatening rhythm called torsades de pointes goes up by 5.7 times.
Another sneaky one: ACE inhibitors (like lisinopril) plus potassium-sparing diuretics (like amiloride). Both raise potassium levels. Alone, they’re fine. Together? Potassium can climb by 1.0-1.5 mmol/L. That’s enough to stop your heart.
Who’s at Highest Risk?
It’s not just about the drugs. It’s about the person.
Older adults are the most vulnerable. Why? They often take five or more medications. The Beers Criteria - a guide used by doctors in the US and UK - lists 30 high-risk combinations for people over 65. The top offenders? Anticoagulants, NSAIDs, benzodiazepines, and heart drugs.
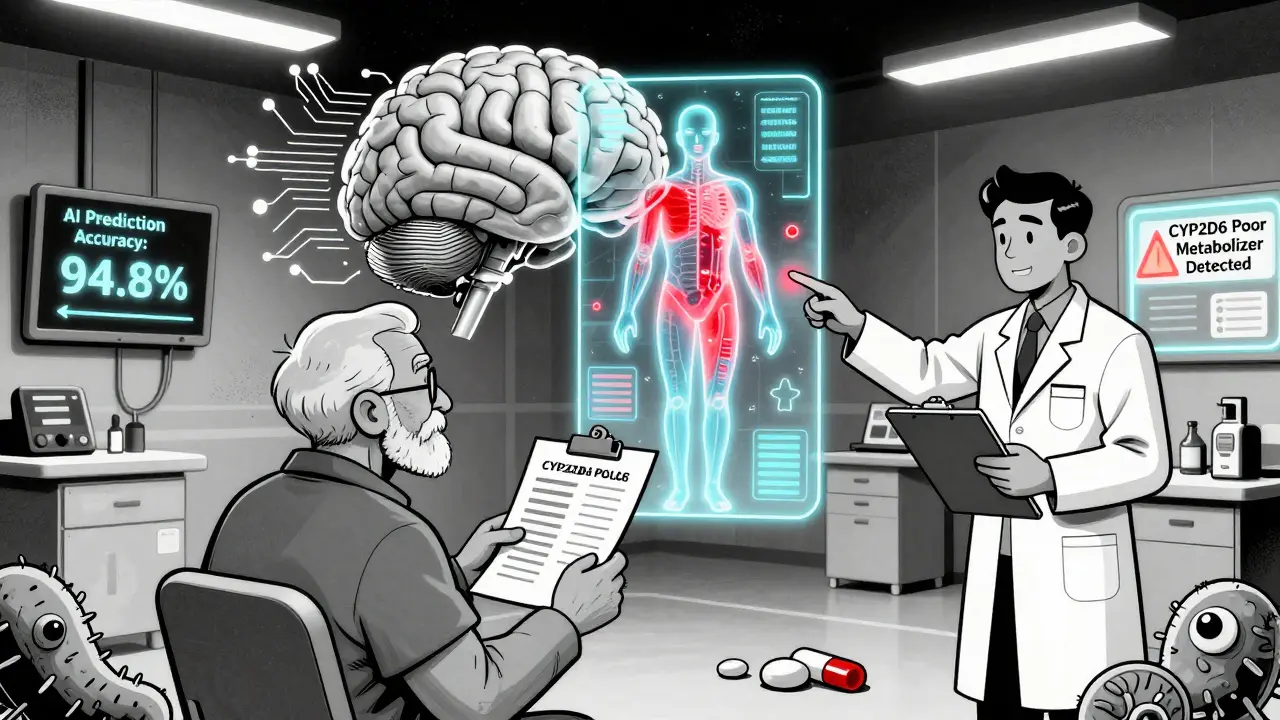
Genetics matter too. About 5-10% of people are poor metabolizers of CYP2D6. That means they can’t convert codeine into morphine properly. But if they’re also taking a CYP3A4 inhibitor like fluoxetine? Their body might still make too much morphine - leading to breathing problems. Conversely, ultrarapid metabolizers might get no pain relief from codeine at all.
People with kidney or liver disease are also at higher risk. Their bodies can’t clear drugs the way a healthy person can. Even small doses can pile up.
How Doctors and Pharmacies Try to Prevent This
Electronic health records now have built-in alerts. But here’s the problem: they’re wrong 80-90% of the time. That’s called alert fatigue. Doctors start ignoring them.
Pharmacists are the unsung heroes here. A 2021 study showed that when pharmacists reviewed patients’ full medication lists, they cut dangerous interactions by 37%. That’s not magic. It’s just asking: “What are you taking? Why? Have you been told not to mix these?”
Specialized tools exist too. The Liverpool HIV-Drug Interactions Checker updates daily and covers over 350 antiretroviral combinations. It’s used by clinics worldwide because HIV meds are especially prone to interactions.
Therapeutic drug monitoring (TDM) helps with drugs like warfarin, lithium, and digoxin. Instead of guessing, doctors measure the actual drug level in your blood. That’s how they know if you’re safe.
What You Can Do
You don’t need to be a scientist to protect yourself.
- Keep a list of every medicine you take - including supplements, vitamins, and herbal products. Don’t forget over-the-counter stuff like ibuprofen or antacids.
- Bring that list to every appointment. Even if you’ve been to the same doctor before.
- Ask: “Could this new medicine interact with anything else I’m taking?”
- If you’re on warfarin, watch your vitamin K intake. Leafy greens are healthy, but they can make warfarin less effective.
- Don’t start St. John’s Wort or grapefruit juice without checking. Grapefruit blocks CYP3A4. It can turn a safe dose of a statin into a dangerous one.
The Future: Personalized Medicine and AI
The next big leap isn’t just about avoiding bad combos. It’s about predicting them before you even take the first pill.
Pharmacogenomics - testing your genes to see how you metabolize drugs - is becoming more common. The Clinical Pharmacogenetics Implementation Consortium (CPIC) has published 22 guidelines that tell doctors what to do based on your DNA. For example: if you’re a CYP2D6 ultrarapid metabolizer, avoid codeine entirely.
Artificial intelligence is stepping in too. A 2021 study trained an AI on 89 million electronic health records. It predicted dangerous drug interactions with 94.8% accuracy - far better than old rule-based systems. These tools are starting to appear in hospital systems like Epic, reducing severe interactions by 22% in real-world use.
And research is moving fast. Scientists are now studying how your gut bacteria affect drug metabolism. One study found that certain bacteria can break down digoxin before it even enters your bloodstream. That could explain why some people don’t respond to the drug - even when their blood levels look normal.
Why This Matters
Drug interactions aren’t just a medical footnote. They cost the US healthcare system $1.3 billion a year - mostly from hospital stays caused by bleeding, muscle damage, or heart problems. Many of these are preventable.
It’s not about fear. It’s about awareness. Every pill you take has a story. And sometimes, when two stories meet, they don’t end the way you expect.
Know your meds. Ask questions. Don’t assume something is safe just because it’s over the counter or natural. The body doesn’t care where the drug came from. It only cares what it does - and who else is in the room with it.
What are the most common dangerous drug interactions?
The most dangerous and frequently reported interactions involve warfarin (with NSAIDs, antibiotics, or St. John’s Wort), statins (especially simvastatin with ketoconazole or grapefruit juice), and combinations that prolong the QT interval like macrolides with fluoroquinolones. Also common are ACE inhibitors with potassium-sparing diuretics, which can cause life-threatening hyperkalemia.
Can herbal supplements cause drug interactions?
Yes. St. John’s Wort is one of the most potent - it induces CYP3A4 and P-gp, reducing levels of birth control pills, antidepressants, and transplant drugs like cyclosporine. Garlic, ginkgo, and ginger can also thin the blood and increase bleeding risk when taken with warfarin or aspirin. Many people assume ‘natural’ means safe, but that’s not true.
Why do some people have worse interactions than others?
Genetics play a big role. Variations in CYP enzymes mean some people metabolize drugs very slowly (poor metabolizers) or extremely fast (ultrarapid metabolizers). Age, liver or kidney disease, and even diet (like grapefruit or high-vitamin K foods) also change how your body handles drugs. It’s not just the drugs - it’s you.
Are drug interactions more common in older adults?
Yes. People over 65 are at highest risk because they often take five or more medications. Studies show drug interactions cause 3-5% of hospital admissions in this group. The Beers Criteria lists 30 high-risk combinations specifically for older adults, including NSAIDs with anticoagulants and benzodiazepines with opioids.
Can electronic health records prevent all drug interactions?
No. Current systems have a false alert rate of 80-90%. Clinicians often ignore them because they’re too noisy. That’s why pharmacist-led reviews and patient education are still the most effective tools. Newer AI-driven systems are improving, but they’re not perfect yet.
How do I know if my meds are interacting?
Watch for new or worsening symptoms after starting a new drug - like unexplained bruising, muscle pain, dizziness, irregular heartbeat, or extreme fatigue. If you notice anything unusual, don’t wait. Contact your doctor or pharmacist. Blood tests (like INR for warfarin or creatinine for kidney function) can also show if something’s off.

Comments (12)
clarissa sulio
February 1, 2026 AT 16:43This is why we need to stop letting big pharma push drugs without proper testing. People die because doctors don't know what's in these pills. I've seen it firsthand. No more shortcuts.
Ansley Mayson
February 1, 2026 AT 22:03Most of these interactions are avoidable if you just read the damn label
Marc Durocher
February 3, 2026 AT 11:09I love how we treat medicine like it's a video game where you just stack buffs and debuffs. Your liver isn't a NPC. It's a tired 90-year-old janitor trying to clean up after a frat party.
Nick Flake
February 4, 2026 AT 22:59Every pill you swallow is a conversation between your body and a chemical stranger 🌍💊. Some of these conversations are polite. Others? They end in screaming matches and ER visits. We need to listen better.
Akhona Myeki
February 6, 2026 AT 08:15The CYP450 system is not a suggestion. It is a biological law. Anyone who takes St. John's Wort with prescription medication is playing Russian roulette with their organs. This is not debate worthy.
Chinmoy Kumar
February 7, 2026 AT 11:13i never knew grapefruit could mess with statins like that wow i always thought natural meant safe but now i see its more like natural but dangerous lol
Bridget Molokomme
February 7, 2026 AT 22:27So let me get this straight... you're telling me my ibuprofen and warfarin combo is basically me holding a lit match to my own veins? Cool. Thanks for the heads up.
Vatsal Srivastava
February 9, 2026 AT 21:49The whole pharmacokinetic model is outdated. We've known for years that gut microbiome plays a bigger role than liver enzymes. This article is 2010 thinking in 2024
Bob Hynes
February 11, 2026 AT 13:11I live in Canada and we have way better med reviews here. Pharmacists actually call you if they see a bad combo. In the US it's just 'here's your script, good luck'
Brittany Marioni
February 12, 2026 AT 16:53I cannot believe how many people still don't realize that supplements are drugs too! They are not 'just herbs'-they are potent, bioactive compounds that interact with your system. Please, please, please-keep a list! Write it down! Use a notebook! Don't rely on your memory!
Eli Kiseop
February 12, 2026 AT 21:03I started taking omeprazole and then my antidepressant stopped working and I didn't connect the dots until my doctor said hey maybe its the acid blocker
Ellie Norris
February 14, 2026 AT 12:55I'm a pharmacist and I can say this: the single biggest thing patients miss is that even 'harmless' things like turmeric or magnesium can interfere. Always tell us everything. Even the stuff you think is too small to mention.