For someone living with Parkinson’s disease, nausea isn’t just an inconvenience-it’s a daily battle. Up to 80% of patients experience nausea when starting levodopa, the mainstay treatment for Parkinson’s. But here’s the catch: the very drugs doctors reach for to stop that nausea can make Parkinson’s symptoms worse. This isn’t a rare side effect. It’s a well-documented, dangerous interaction that still catches many patients and even some doctors off guard.
Why Dopamine Blockers Are a Problem
Parkinson’s disease is caused by the slow death of dopamine-producing neurons in the brain. Levodopa replaces that lost dopamine, helping patients move more smoothly. But many antiemetics-drugs meant to stop nausea-work by blocking dopamine receptors. That sounds helpful, right? Wrong. In a brain already starved of dopamine, blocking what’s left can trigger or worsen tremors, stiffness, freezing, and slow movement. The problem isn’t just theoretical. It’s clinical, common, and often avoidable. Drugs like metoclopramide (Reglan), prochlorperazine (Stemetil), and haloperidol (Haldol) are all dopamine D2-receptor antagonists. They work in the gut and brain to stop vomiting. But when they cross the blood-brain barrier, they interfere with levodopa’s effect. The result? A patient who was stable one day can wake up unable to walk the next.Not All Antiemetics Are Created Equal
The key difference between safe and dangerous antiemetics comes down to one thing: whether they enter the brain. Metoclopramide crosses the blood-brain barrier easily-about 20-40% of the dose gets in. That’s why it’s been linked to acute dystonia and worsening Parkinsonism in studies dating back to 1971. Even though it has some serotonin-boosting effects that might slightly balance its risks, the American Parkinson Disease Association still lists it as a medication to avoid. Patients on forums like Parkinson’s UK and Reddit report dramatic worsening of symptoms after even a single dose. Domperidone (Motilium) is different. It barely crosses into the brain-less than 5%-because of a natural pump called P-glycoprotein that pushes it back out. That makes it one of the safest antiemetics for Parkinson’s patients. It works just as well in the gut to stop nausea, but leaves the brain’s dopamine alone. The catch? It’s not available as an injection in the U.S., and the FDA restricts its oral form due to heart rhythm concerns in older adults. But for Parkinson’s patients, the risk of worsening motor symptoms is under 2%. Cyclizine (Vertin) is another option. It doesn’t block dopamine at all. Instead, it targets histamine receptors. That’s why its risk of worsening Parkinson’s is only 5-10%. It’s often the first choice in UK guidelines. Ondansetron (Zofran) blocks serotonin, not dopamine, so it’s generally safer too-though some patients find it less effective for levodopa-induced nausea.What Doctors Still Get Wrong
Despite decades of research, this interaction remains a blind spot. A 2022 study found only 37% of emergency room doctors knew metoclopramide was dangerous for Parkinson’s patients. In hospitals, it’s still routinely given for post-op nausea or chemotherapy side effects-even when the patient has Parkinson’s. Patients report being given prochlorperazine in A&E after vomiting, only to be left stuck in bed with severe rigidity. One man on the Parkinson’s NSW Forum said his tremors spiked after a dental procedure and took three weeks to settle, even after increasing his levodopa dose. That’s not just frustrating-it’s dangerous. Worsening symptoms can lead to falls, hospitalization, and longer recovery. The Michael J. Fox Foundation’s 2022 survey found that 68% of Parkinson’s patients who received dopamine-blocking antiemetics in hospital saw their motor symptoms worsen. Over 20% needed extended stays. Meanwhile, 85% of those who took domperidone reported no negative effects.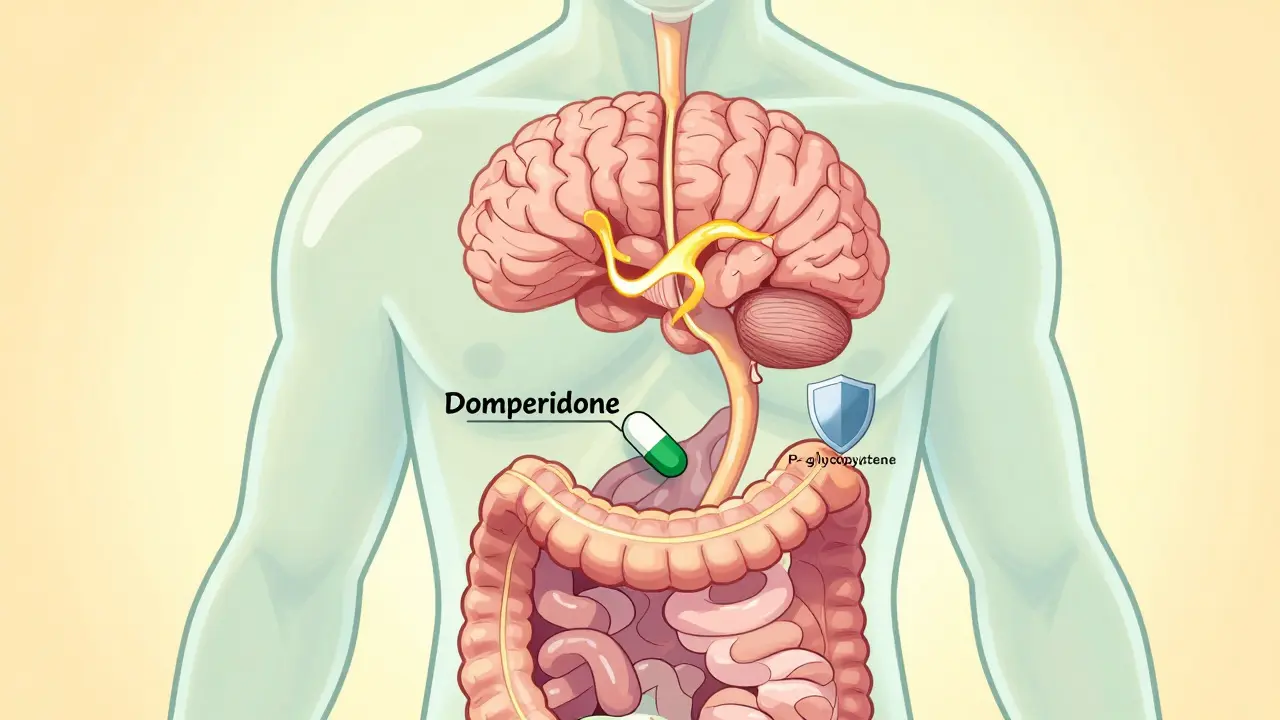
What to Use Instead
If you have Parkinson’s and struggle with nausea, here’s what works-and what doesn’t.- First-line: Cyclizine - Low risk, widely available, effective for many. Start with 25-50mg up to three times a day.
- Second-line: Domperidone - Best for persistent nausea. Requires prescription and monitoring for heart rhythm, especially if you’re over 60 or on other heart medications.
- Third-line: Ondansetron - Good for chemotherapy or post-op nausea. Less reliable for levodopa-related nausea, but still safer than dopamine blockers.
- Emerging option: Aprepitant - A newer drug that blocks a different nausea pathway. In a 2023 trial, it controlled nausea in 92% of Parkinson’s patients with zero motor side effects.
Non-Drug Strategies Work Too
Before reaching for pills, try these simple, evidence-backed approaches:- Ginger - Take 1 gram daily in capsule or tea form. Studies show it reduces nausea without affecting dopamine.
- Small, frequent meals - Large meals slow stomach emptying, which worsens nausea. Eating six small meals a day helps.
- Stay hydrated - Dehydration makes nausea worse. Sip water or electrolyte drinks slowly.
- Take levodopa on an empty stomach - Wait 30-60 minutes before or after eating. Protein interferes with levodopa absorption, which can make nausea worse.

Red Flags: When to Say No
If a doctor prescribes any of these, ask for an alternative:- Metoclopramide (Reglan, Maxalon)
- Prochlorperazine (Stemetil)
- Haloperidol (Haldol)
- Chlorpromazine
- Promethazine (Phenergan)
- Droperidol
What About Antipsychotics?
Some Parkinson’s patients develop hallucinations or psychosis later in the disease. When that happens, doctors may consider antipsychotics. But most traditional ones-like risperidone or olanzapine-also block dopamine and can be devastating. The only antipsychotics considered safe for Parkinson’s are:- Clozapine (Clozaril)
- Quetiapine (Seroquel)
- Pimavanserin (Nuplazid)
What You Can Do Right Now
If you or a loved one has Parkinson’s:- Ask your neurologist for a list of safe antiemetics. Keep it in your wallet.
- Carry a Parkinson’s Medication Safety Card (available from APDA or Parkinson’s UK). These cards list dangerous drugs and have been shown to reduce bad prescriptions by 40%.
- Never accept a new antiemetic without checking its mechanism. If it says “dopamine antagonist” or “D2 blocker,” say no.
- If you’ve been given metoclopramide or prochlorperazine and your symptoms worsened, tell your doctor immediately. Document it.
- Request domperidone or cyclizine as your first option for nausea.
There’s been progress. In the UK, the MHRA issued a formal warning about metoclopramide in Parkinson’s patients in 2019. The Parkinson’s Foundation trained over 1,200 providers in 2023, cutting inappropriate prescriptions by 55% in participating hospitals. But the problem isn’t solved. Too many patients still get the wrong drug.
Managing nausea in Parkinson’s isn’t about choosing between comfort and control. It’s about finding the right tools-ones that don’t trade one problem for another. The science is clear. The alternatives exist. What’s missing is awareness. Don’t let a simple nausea pill undo months of progress.
Can I take metoclopramide if I have Parkinson’s disease?
No. Metoclopramide is a dopamine D2 receptor antagonist and crosses the blood-brain barrier. It can cause sudden worsening of tremors, stiffness, and slowness in Parkinson’s patients. The American Parkinson Disease Association and UK’s MHRA both warn against its use. Even if it was given to you before without issues, the risk increases over time and with higher doses.
Is domperidone safe for Parkinson’s patients?
Yes, domperidone is generally considered the safest antiemetic for Parkinson’s patients because it doesn’t cross the blood-brain barrier significantly. It works in the gut to stop nausea without affecting brain dopamine. However, it carries a small risk of heart rhythm changes, especially in people over 60 or those taking other medications that affect the heart. Always use the lowest effective dose and get regular ECG checks if you’re on it long-term.
What should I do if I was given metoclopramide in the hospital?
If you notice your tremors, stiffness, or freezing getting worse after receiving metoclopramide, contact your neurologist immediately. Do not wait. You may need to increase your levodopa dose temporarily under medical supervision. Document the incident and ask for a note in your medical record. Consider carrying a Parkinson’s Medication Safety Card to prevent this from happening again.
Are there any over-the-counter antiemetics I can use?
Avoid all OTC antiemetics unless you’ve confirmed they’re safe. Many contain dimenhydrinate (Dramamine) or meclizine, which have anticholinergic effects and can worsen confusion or urinary retention in Parkinson’s. Ginger supplements are safe and effective as a natural option. Cyclizine is available over the counter in some countries like the UK, but always check with your doctor first.
Why don’t doctors know this?
Many doctors, especially in emergency rooms or non-neurology specialties, aren’t trained in Parkinson’s-specific medication risks. Antiemetics like metoclopramide are standard for nausea in general medicine. The interaction isn’t always taught in medical school, and drug databases don’t always flag it clearly. That’s why patient advocacy-like carrying a safety card-is so important.
Can I use ginger instead of medication?
Yes. Ginger is one of the most effective non-drug options. Studies show 1 gram of ginger daily (in capsule or tea form) reduces nausea in Parkinson’s patients with no side effects. It doesn’t interfere with levodopa or dopamine pathways. Try it before reaching for pills. Combine it with small, frequent meals and staying hydrated for best results.
What if I need an antiemetic for chemotherapy?
If you have Parkinson’s and need chemo, tell your oncologist upfront. Ondansetron is often used for chemo nausea and is generally safe. Aprepitant (Emend) is newer and highly effective with no known impact on motor symptoms. Avoid dopamine blockers like prochlorperazine or metoclopramide at all costs. A coordinated care plan between your neurologist and oncologist is essential.


Comments (11)
Hank Pannell
January 3, 2026 AT 19:30It's fascinating how the blood-brain barrier acts as a biological gatekeeper-domperidone’s P-glycoprotein efflux is a perfect example of evolutionary pharmacology in action. We’re not just treating symptoms; we’re navigating neurochemical topography. The fact that a molecule can be structurally identical to a neurotoxin yet remain inert in the CNS due to transporter biology… that’s elegance. It’s not just about avoiding dopamine antagonists-it’s about understanding the architecture of neural access.
And yet, why is this still not standard curriculum in med schools? The 2022 ER study showing only 37% awareness is a systemic failure, not a knowledge gap. We’ve mapped the human genome but still treat Parkinson’s like a generic GI disorder. The disconnect between molecular mechanism and clinical practice is staggering.
Apripitant’s 92% efficacy in 2023 trials? That’s not a breakthrough-it’s a long-overdue correction. We’re finally moving from symptom suppression to pathway-specific modulation. The real tragedy isn’t metoclopramide-it’s that we’ve spent 50 years treating Parkinson’s nausea with the wrong tool because we didn’t ask ‘how does this cross the BBB?’
And don’t get me started on the FDA’s heart rhythm restrictions on domperidone. We’re risking cardiac arrhythmias in 0.5% of elderly patients to prevent a 2% risk of catastrophic motor decline. That’s not risk management-it’s institutional inertia dressed as caution.
Neurology needs a paradigm shift: no drug should be prescribed for a Parkinson’s patient without a BBB permeability audit. We need mandatory pharmacogenomic flags in EHRs. This isn’t niche-it’s foundational.
Ian Ring
January 4, 2026 AT 13:33Domperidone is the gold standard, honestly. I’ve been on it for 4 years now-Parkinson’s + chronic nausea-and it’s been life-changing. No tremor spikes, no rigidity, just… normal. I wish it were easier to get here in the UK; my GP had to jump through hoops just to prescribe it. But it’s worth it. Ginger tea in the morning, domperidone at lunch, and I can actually eat without feeling like I’m going to hurl. <3
erica yabut
January 5, 2026 AT 23:58Oh, so now we’re treating Parkinson’s like a boutique wellness brand? Ginger tea? Small meals? How quaint. Meanwhile, real medicine-pharmacology, molecular targeting, clinical trials-is being replaced by Pinterest-approved ‘natural remedies.’ If you want to cure nausea with turmeric and intention, go to a yoga retreat. But if you’re actually sick, you need science-not hippie rituals masquerading as evidence.
And let’s be real: the ‘safety card’ is a gimmick for people who can’t read a drug label. If your doctor doesn’t know metoclopramide is contraindicated, they shouldn’t be prescribing anything. Blame the system? Sure. But don’t pretend carrying a laminated card makes you an expert.
Kerry Howarth
January 7, 2026 AT 12:49Domperidone works. Cyclizine works. Ginger works. Metoclopramide doesn’t. It’s that simple. If you have Parkinson’s, know this list. Print it. Show it to every doctor. No exceptions. This isn’t opinion-it’s clinical fact. Your movement matters.
Joy F
January 8, 2026 AT 08:27Okay, but what if you’re the one who got stuck in the hospital for three weeks after they gave you Reglan? What if you woke up paralyzed, your husband screaming at the nurses, and no one believed you when you said, ‘I have Parkinson’s’? What if your meds were increased, your insurance denied domperidone, and you had to beg your neurologist to fight for you? This isn’t just ‘awareness.’ This is trauma. This is the quiet horror of being treated like a statistic until your body breaks.
I used to be a dancer. Now I need a walker. And it wasn’t the disease. It was the damn antiemetic.
So yeah. Carry the card. Yell at the ER. Send emails to the FDA. Because if you don’t, someone else’s mother will end up in a wheelchair because a resident thought ‘nausea is nausea.’
Haley Parizo
January 9, 2026 AT 05:57Let’s not romanticize domperidone. It’s not a miracle-it’s a compromise. The FDA restricted it because it causes QT prolongation. And yes, the motor risk is low, but cardiac risk isn’t zero. We’re trading one life-threatening side effect for another. That’s not safety-that’s risk redistribution.
And why is aprepitant so expensive? Because Big Pharma knows we’re desperate. They’ve cornered the market on non-dopaminergic antiemetics and priced it like a luxury good. Meanwhile, cyclizine, a 1950s antihistamine, is the unsung hero. Why aren’t we pushing for generic reformulation? Why aren’t we demanding cheaper access to aprepitant? Because the system doesn’t care about Parkinson’s patients-it cares about profit margins.
This isn’t medicine. It’s a moral crisis wrapped in a clinical guideline.
Brittany Wallace
January 9, 2026 AT 07:29I love how this thread is turning into a masterclass in neuropharmacology. I’m a caregiver, not a doctor, but I’ve learned more in the last year than I did in med school. Domperidone saved my mom’s quality of life. We started with ginger, then cyclizine, then domperidone. Each step felt like reclaiming a piece of her. And honestly? The fact that we even have options is a win. We’re not just surviving-we’re adapting. <3
Liam Tanner
January 10, 2026 AT 11:04For anyone new to this: don’t panic. You don’t need to memorize every drug name. Just remember: if it ends in ‘-prazole’ or ‘-perazine’ or ‘-pride’, check it. If it says ‘dopamine antagonist’ on the sheet, say no. Ask for cyclizine or domperidone. If they say ‘we don’t have that,’ ask why. And if they still say no-ask for the pharmacy director. You have a right to safe care. This isn’t optional.
veronica guillen giles
January 10, 2026 AT 22:21Oh wow. So the answer to ‘why do doctors keep messing up?’ is… carry a card? That’s it? You’re telling me the entire healthcare system’s failure to train ER staff on Parkinson’s meds is solved by a laminated piece of paper? How cute. I bet the next suggestion is ‘wear a t-shirt that says I HAVE PARKINSON’S.’
Meanwhile, in the real world, hospitals still give metoclopramide because it’s cheap, fast, and the nurse didn’t read the chart. No one’s going to stop and ask if you have Parkinson’s when you’re vomiting in the ER. The system is broken. Cards won’t fix it. Advocacy won’t fix it. Only policy will.
Vincent Sunio
January 11, 2026 AT 00:39Let’s be precise: domperidone is not ‘safe.’ It is merely less dangerous than metoclopramide. The literature is clear: QT prolongation risk is dose-dependent and cumulative. The FDA’s restriction is not arbitrary-it is evidence-based. To claim domperidone is ‘the best option’ is a misrepresentation of risk-benefit analysis. Furthermore, aprepitant’s 92% efficacy was observed in a small, non-diverse cohort. Extrapolation to the broader Parkinson’s population is premature.
And ginger? A 2017 Cochrane review found only marginal benefit over placebo for chemotherapy-induced nausea. To elevate it to first-line status in Parkinson’s is pseudoscientific. This post reads like a wellness blog masquerading as clinical guidance.
JUNE OHM
January 12, 2026 AT 05:15THIS IS A BIG PHARMA COVER-UP. THEY WANT YOU TO USE DOMPERIDONE BECAUSE IT'S EXPENSIVE AND THEY OWN THE PATENT. METOCLOPRAMIDE IS CHEAPER AND THEY MAKE BILLIONS OFF IT. THE FDA IS IN BED WITH BIG PHARMA. THEY DON'T WANT YOU TO KNOW THAT GINGER AND CUCUMBER WATER CAN CURE PARKINSON'S NAUSEA. I SAW A VIDEO ON TIKTOK WHERE A WOMAN WITH PARKINSON'S STOPPED ALL MEDS AND JUST DRANK CUCUMBER WATER FOR 30 DAYS AND WALKED AGAIN. THEY'RE HIDING THE TRUTH. #SaveParkinsons #BigPharmaLies